Main Model
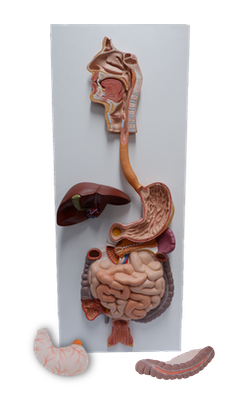
Jejunum

Jejunum and Ileum
The second part of the small intestine, the jejunum, begins at the duodenojejunal flexure where the gastrointestinal tract resumes an intraperitoneal course. The third part of the small intestine, the ileum, ends at the ileocecal junction, the union of the terminal ileum and the cecum. Together, the jejunum and ileum are 6-7 m long, the jejunum constituting approximately two fifths and the ileum approximately three fifths of the intraperitoneal section of the small intestine.
Most of the jejunum lies in the left upper quadrant (LUQ) of the infracolic compartment, whereas most of the ileum lies in the right lower quadrant (RLQ). The terminal ileum usually lies in the pelvis from which it ascends, ending in the medial aspect of the cecum. Although no clear line of demarcation between the jejunum and ileum exists, they have distinctive characteristics that are surgically important.
The mesentery is a fan-shaped fold of peritoneum that attaches the jejunum and ileum to the posterior abdominal wall. The origin or root of the mesentery (approximately 15 cm long) is directed obliquely, inferiorly, and to the right. It extends from the duodenojejunal junction on the left side of vertebra L2to the ileocolic junction and the right sacro-iliac joint. The average length of the mesentery from its root to the intestinal border is 20 cm. The root of the mesentery crosses (successively) the ascending and inferior parts of the duodenum, abdominal aorta, IVC, right ureter, right psoas major, and right testicular or ovarian vessels. Between the two layers of the mesentery are the superior mesenteric vessels, lymph nodes, a variable amount of fat, and autonomic nerves.
The superior mesenteric artery (SMA) supplies the jejunum and ileum via jejunal and ileal arteries.
The SMA usually arises from the abdominal aorta at the level of the L1 vertebra, approximately 1 cm inferior to the celiac trunk, and runs between the layers of the mesentery, sending 15-18 branches to the jejunum and ileum. The arteries unite to form loops or arches, called arterial arcades, which give rise to straight arteries, called vasa recta.
The superior mesenteric vein drains the jejunum and ileum. It lies anterior and to the right of the SMA in the root of the mesentery. The SMV ends posterior to the neck of the pancreas, where it unites with the splenic vein to form the hepatic portal vein.
Specialized lymphatic vessels in the intestinal villi (tiny projections of the mucous membrane) that absorb fat are called lacteals. They empty their milk-like fluid into the lymphatic plexuses in the walls of the jejunum and ileum. The lacteals drain in turn into lymphatic vessels between the layers of the mesentery. Within the mesentery, the lymph passes sequentially through three groups of lymph nodes:
• Juxta-intestinal lymph nodes: located close to the intestinal wall.
• Mesenteric lymph nodes: scattered among the arterial arcades.
• Superior central nodes: located along the proximal part of the SMA.
Efferent lymphatic vessels from the mesenteric lymph nodes drain to the superior mesenteric lymph nodes. Lymphatic vessels from the terminal ileum follow the ileal branch of the ileocolic artery to the ileocolic lymph nodes.
The SMA and its branches are surrounded by a peri-arterial nerve plexus through which the nerves are conducted to the parts of the intestine supplied by this artery. The sympathetic fibers in the nerves to the jejunum and ileum originate in the T8-T10 segments of the spinal cord and reach the superior mesenteric nerve plexus through the sympathetic trunks and thoracic abdominopelvic (greater, lesser, and least) splanchnic nerves. The presynaptic sympathetic fibers synapse on cell bodies of postsynaptic sympathetic neurons in the celiac and superior mesenteric (prevertebral) ganglia. The parasympathetic fibers in the nerves to the jejunum and ileum derive from the posterior vagal trunks. The presynaptic parasympathetic fibers synapse with postsynaptic parasympathetic neurons in the myenteric and submucosal plexuses in the intestinal wall.
Sympathetic stimulation reduces peristaltic and secretory activity of the intestine and acts as a vasoconstrictor, reducing or stopping digestion and making blood (and energy) available for "fleeing or fighting." Parasympathetic stimulation increases peristaltic and secretory activity of the intestine, restoring the digestion process following a sympathetic reaction. The small intestine also has sensory (visceral afferent) fibers. The intestine is insensitive to most pain stimuli, including cutting and burning; however, it is sensitive to distension that is perceived as colic (spasmodic abdominal pains or "intestinal cramps").