Main Model
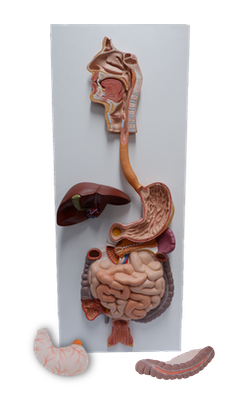
Esophagus

The esophagus is a muscular tube (approximately 25 cm [10 inches] long) with an average diameter of 2 cm that conveys food from the pharynx to the stomach. As seen during fluoroscopy (x-ray, using a fluoroscope) after a barium swallow, the esophagus normally has three constrictions where adjacent structures produce impressions:
• Cervical constriction (upper esophageal sphincter): at its beginning at the pharyngoesophageal junction, approximately 15 cm from the incisor teeth; caused by the cricopharyngeus muscle.
• Thoracic (broncho-aortic) constriction: a compound constriction where it is first crossed by the arch of the aorta, 22.5 cm from the incisor teeth, and then where it is crossed by the left main bronchus, 27.5 cm from the incisor teeth; the former is seen in anteroposterior views, the latter in lateral views.
• Diaphragmatic constriction: where it passes through the esophageal hiatus of the diaphragm, approximately 40 cm from the incisor teeth.
Awareness of these constrictions is important when passing instruments through the esophagus into the stomach, and when viewing radiographs of patients who are experiencing dysphagia (difficulty in swallowing).
The esophagus:
• Follows the curve of the vertebral column as it descends through the neck and mediastinum - the median partition of the thoracic cavity.
• Has internal circular and external longitudinal layers of muscle. In its superior third, the external layer consists of voluntary striated muscle; the inferior third is composed of smooth muscle, and the middle third is made up of both types of muscle.
• Passes through the elliptical esophageal hiatus in the muscular right crus of the diaphragm, just to the left of the median plane at the level of the T10 vertebra.
• Terminates by entering the stomach at the cardial orifice of the stomach to the left of the midline at the level of the 7th left costal cartilage and T11 vertebra.
• Is encircled by the esophageal (nerve) plexus distally.
Food passes through the esophagus rapidly because of the peristaltic action of its musculature, aided by but not dependent on gravity (one can still swallow if inverted). The esophagus is attached to the margins of the esophageal hiatus in the diaphragm by the phrenico-esophageal ligament, an extension of inferior diaphragmatic fascia. This ligament permits independent movement of the diaphragm and esophagus during respiration and swallowing.
The trumpet-shaped abdominal part of the esophagus, only 1.25 cm long, passes from the esophageal hiatus in the right crus of the diaphragm to the cardial orifice of the stomach, widening as it approaches, passing anteriorly and to the left as it descends inferiorly. Its anterior surface is covered with peritoneum of the greater sac, continuous with that covering the anterior surface of the stomach. It fits into a groove on the posterior (visceral) surface of the liver.
The posterior surface of the abdominal part of the esophagus is covered with peritoneum of the omental bursa, continuous with that covering the posterior surface of the stomach. The right border of the abdominal esophagus is continuous with the lesser curvature of the stomach; however, its left border is separated from the fundus of the stomach by the cardial notch between the esophagus and fundus.
The esophagogastric junction lies to the left of the T11 vertebra on the horizontal plane that passes through the tip of the xiphoid process. Surgeons and endoscopists designate the Z-line, a jagged line where the mucosa abruptly changes from esophageal to gastric mucosa, as the junction. Immediately superior to this junction, the diaphragmatic musculature forming the esophageal hiatus functions as a physiological inferior esophageal sphincter that contracts and relaxes. Radiologic studies show that food stops here momentarily and that the sphincter mechanism is normally efficient in preventing reflux of gastric contents into the esophagus. When one is not eating, the lumen of the esophagus is normally collapsed superior to this level to prevent food or stomach juices from regurgitating into the esophagus.
The arterial supply of the abdominal part of the esophagus is from the left gastric artery, a branch of the celiac trunk, and the left inferior phrenic artery.
The venous drainage from the submucosal veins of this part of the esophagus is both to the portal venous system through the left gastric vein and into the systemic venous system through esophageal veins entering the azygos vein.
The lymphatic drainage of the abdominal part of the esophagus is into the left gastric lymph nodes; efferent lymphatic vessels from these nodes drain mainly to celiac lymph nodes.
The esophagus is innervated by the esophageal plexus, formed by the vagal trunks (becoming anterior and posterior gastric branches), and the thoracic sympathetic trunks via the greater (abdominopelvic) splanchnic nerves and periarterial plexuses around the left gastric and inferior phrenic arteries.