Main Model

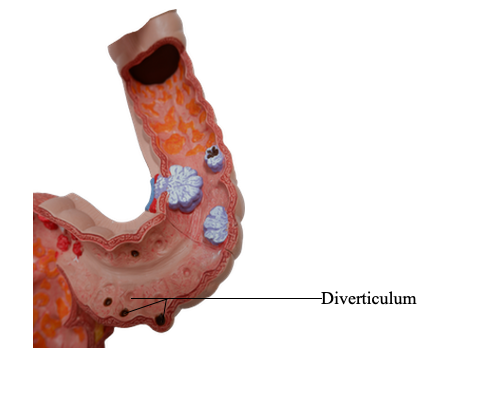
Diverticulum
Inflammatory Intestinal Disease
Sigmoid Diverticulitis
In general, diverticular disease refers to acquired pseudodiverticular outpouchings of the colonic mucosa and submucosa. Such colonic diverticula are rare in individuals
younger than 30 years of age, but the prevalence approaches
50% in Western adult populations older than 60 years of
age. Diverticula generally are multiple, and the condition
is referred to as diverticulosis. This disease is much less
common in developing countries, probably because of dietary differences.
Pathogenesis
Colonic diverticula tend to develop under conditions of
elevated intraluminal pressure in the sigmoid colon. This
is facilitated by the unique structure of the colonic muscularis propria, where nerves, arterial vasa recta, and their
connective tissue sheaths penetrate the inner circular
muscle coat to create discontinuities in the muscle wall. In
other parts of the intestine, these gaps are reinforced by the
external longitudinal layer of the muscularis propria, but
in the colon, this muscle layer is discontinuous, being gathered into three bands termed taeniae coli. High luminal
pressures may be generated by exaggerated peristaltic contractions, with spasmodic sequestration of bowel segments
that may be exacerbated by diets low in fiber, which reduce
stool bulk.
Morphology
Anatomically, colonic diverticula are small, flasklike outpouchings,
usually 0.5 to 1 cm in diameter, that occur in a regular distribution in between the taeniae coli. They are
most common in the sigmoid colon, but other regions of the
colon may be affected. Colonic diverticula have a thin wall composed of a flattened or atrophic mucosa, compressed submucosa,
and attenuated muscularis propria - often, this last component
is totally absent. Obstruction of diverticula
with stasis of contents, leads to inflammatory changes, producing diverticulitis and peridiverticulitis. Because the wall of the
diverticulum is supported only by the muscularis mucosa and a
thin layer of subserosal adipose tissue, inflammation, increased pressure, and mucosal ucleration within an obstructed diverticulum can readily result in perforation. With or without perforation, recurrent diverticulitis may cause segmental colitis, fibrotic
thickening in and around the colonic wall, or stricture formation.
Clinical Features
Most individuals with diverticular disease remain asymptomatic throughout their lives. About 20% of those affected develop complaints including intermittent cramping, continuous lower abdominal discomfort, constipation, and
diarrhea. Longitudinal studies have shown that while diverticula can regress early in their development they
often become more numerous and larger over time.
Whether a high-fiber diet prevents such progression or
protects against diverticulitis is unclear. Even when diverticulitis occurs, it most often resolves spontaneously or after antibiotic treatment, and relatively few patients
require surgical intervention.