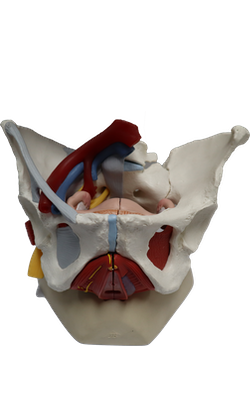
Main Model
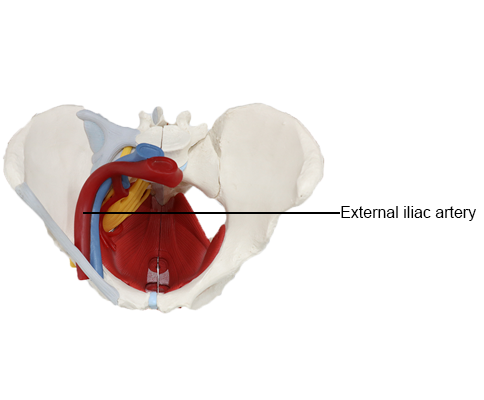
ARTERIES : External iliac artery
Vessels of Posterior Abdominal Wall
The major neurovascular bundle of the inferior trunk, including the abdominal aorta, the inferior vena cava, and the aortic
peri-arterial nerve plexus, courses in the midline of the posterior abdominal wall, anterior to the bodies of the lumbar
vertebrae.
Abdominal Aorta
Most arteries supplying the posterior abdominal wall arise
from the abdominal aorta. The subcostal arteries arise from the thoracic aorta and distribute
inferior to the 12th rib. The abdominal aorta is approximately 13 cm in length. It begins at the aortic hiatus in the diaphragm at the level of the T12 vertebra and ends at the
level of the L4 vertebra by dividing into the right and left common iliac arteries. The abdominal aorta may be represented
on the anterior abdominal wall by a band (approximately 2
cm wide) extending from a median point, approximately 2.5
cm superior to the transpyloric plane to a point slightly (2-3
cm) inferior to and to the left of the umbilicus at the level of
the supracristal plane (plane of the highest points of the iliac
crests). In children and lean adults, the lower abdominal aorta is sufficiently close to the anterior abdominal wall that its pulsations may be detected or apparent when
the wall is relaxed.
The common iliac arteries diverge and run inferolaterally, following the medial border of the psoas muscles to the
pelvic brim. Here each common iliac artery divides into the
internal and external iliac arteries. The internal iliac artery enters the pelvis. The external iliac artery follows the iliopsoas muscle. Just before leaving the abdomen, the external iliac artery gives rise to the inferior epigastric and deep circumflex iliac
arteries, which supply the anterolateral abdominal wall.
Relations of Abdominal Aorta
From superior to
inferior, the important anterior relations of the abdominal
aorta are the:
• Celiac plexus and ganglion.
• Body of the pancreas and splenic vein.
• Left renal vein.
• Horizontal part of the duodenum.
• Coils of small intestine.
The abdominal aorta descends anterior to the bodies of the
T12-L4 vertebrae. The left lumbar veins pass
posterior to the aorta to reach the IVC. On the
right, the aorta is related to the azygos vein, cisterna chyli,
thoracic duct, right crus of the diaphragm, and right celiac
ganglion. On the left, the aorta is related to the left crus of
the diaphragm and the left celiac ganglion.
Branches of the Abdominal Aorta
The branches
of the descending (thoracic and abdominal) aorta may be
described as arising and coursing in three "vascular planes" and can be classified as being visceral or parietal and paired
or unpaired. Paired parietal
branches of the aorta serve the diaphragm and posterior abdominal wall.
The median sacral artery, an unpaired parietal branch,
may be said to occupy a fourth (posterior) plane because it
arises from the posterior aspect of the aorta just proximal to
its bifurcation. Although markedly smaller, it could also be
considered a midline "continuation" of the aorta, in which
case its lateral branches, the small lumbar arteries and lateral sacral branches, would also be included as part of the
paired parietal branches.
Veins of Posterior Abdominal Wall
The veins of the posterior abdominal wall are tributaries of
the IVC, except for the left testicular or ovarian vein, which
enters the left renal vein instead of entering the IVC. The IVC, the largest vein in the body, has no valves
except for a variable, non-functional one at its orifice in the
right atrium of the heart. The IVC returns poorly oxygenated
blood from the lower limbs, most of the back, the abdominal walls, and the abdominopelvic viscera. Blood from the abdominal viscera passes through the portal venous system
and the liver before entering the IVC via the hepatic veins.
The inferior vena cava (IVC) begins anterior to the L5 vertebra by the union of the common iliac veins. The union
occurs approximately 2.5 cm to the right of the median plane,
inferior to the aortic bifurcation and posterior to the proximal
part of the right common iliac artery. The IVC
ascends on the right side of the bodies of the L3-L5 vertebrae and on the right psoas major to the right of the aorta. The IVC leaves the abdomen by passing through the caval
opening in the diaphragm and enters the thorax at the T8 vertebral level. Because it is formed one vertebral level inferior to the aortic bifurcation, and traverses the diaphragm
four vertebral levels superior to the aortic hiatus, the overall
length of the IVC is 7 cm greater than that of the abdominal
aorta, although most of the additional length is intrahepatic.
The IVC collects poorly oxygenated blood from the lower
limbs and non-portal blood from the abdomen and pelvis.
Almost all the blood from the gastrointestinal tract is collected by the hepatic portal system and passes through the
hepatic veins to the IVC.
The tributaries of the IVC correspond to the paired visceral and parietal branches of the abdominal aorta. The
veins that correspond to the unpaired visceral branches of
the aorta are instead tributaries of the hepatic portal vein.
The blood they carry does ultimately enter the IVC via the
hepatic veins, after traversing the liver.
The branches corresponding to the paired visceral
branches of the abdominal aorta include the right suprarenal
vein, the right and left renal veins, and the right gonadal (testicular or ovarian) vein. The left suprarenal and gonadal veins
drain indirectly into the IVC because they are tributaries of
the left renal vein.
Paired parietal branches of the IVC include the inferior
phrenic veins, the 3rd (L3) and 4th (L4) lumbar veins, and
the common iliac veins. The ascending lumbar and azygos
veins connect the IVC and SVC, either directly or indirectly providing collateral pathways.
Lymphatic Vessels and Lymph Nodes of Posterior Abdominal Wall
Lymphatic vessels and lymph nodes lie along the aorta,
IVC, and iliac vessels. The common iliac
lymph nodes receive lymph from the external and internal
iliac lymph nodes. Lymph from the common iliac lymph
nodes passes to the right and left lumbar lymph nodes.
Lymph from the alimentary tract, liver, spleen, and pancreas passes along the celiac and superior and inferior mesenteric arteries to the pre-aortic lymph nodes (celiac and
superior and inferior mesenteric nodes) scattered around
the origins of these arteries from the aorta. Efferent vessels from these nodes form the intestinal lymphatic
trunks, which may be single or multiple, and participate
in the confluence of lymphatic trunks that gives rise to the
thoracic duct.
The right and left lumbar (caval and aortic) lymph nodes
lie on both sides of the IVC and aorta. These nodes receive
lymph directly from the posterior abdominal wall, kidneys,
ureters, testes or ovaries, uterus, and uterine tubes. They
also receive lymph from the descending colon, pelvis, and
lower limbs through the inferior mesenteric and common
iliac lymph nodes. Efferent lymphatic vessels from the large lumbar lymph nodes form the right and left lumbar
lymphatic trunks.
The inferior end of the thoracic duct lies anterior to the
bodies of the L1 and L2 vertebrae between the right crus of
the diaphragm and the aorta. The thoracic duct begins with
the convergence of the main lymphatic ducts of the abdomen, which in only a small proportion of individuals takes
the form of the commonly depicted, thin-walled sac or dilation, the cisterna chyli (chyle cistern). Cisterna chyli vary greatly in size and shape. More often there
is merely a simple or plexiform convergence at this level of
the right and left lumbar lymphatic trunks, the intestinal
lymph trunk(s), and a pair of descending thoracic lymphatic trunks, which carry lymph from the lower six intercostal spaces on each side. Consequently, essentially all the lymphatic drainage from the lower half of the body (deep
lymphatic drainage inferior to the level of the diaphragm
and all superficial drainage inferior to the level of the umbilicus) converges in the abdomen to enter the beginning of
the thoracic duct.
The thoracic duct ascends through the aortic hiatus in
the diaphragm into the posterior mediastinum, where it
collects more parietal and visceral drainage, particularly
from the left upper quadrant of the body. The duct ultimately ends by entering the venous system at the junction
of the left subclavian and internal jugular veins (the left
venous angle).