Main Model
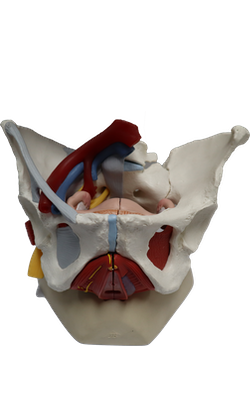
FEMALE INTERNAL GENITAL ORGANS : Fundus of uterus

Uterus
The uterus (womb) is a thick-walled, pear-shaped, hollow muscular organ. The embryo and fetus develop in
the uterus. Its muscular walls adapt to the growth of the
fetus and then provide the power for its expulsion during
childbirth. The non-gravid (non-pregnant) uterus usually
lies in the lesser pelvis, with its body lying on the urinary
bladder and its cervix between the urinary bladder and
rectum.
The uterus is a very dynamic structure, the size and proportions of which change during the various changes of life.
The adult uterus is usually anteverted (tipped anterosuperiorly relative to the axis of the vagina) and anteflexed
(flexed or bent anteriorly relative to the cervix, creating the
angle of flexion) so that its mass lies over the bladder. Consequently, when the bladder is empty, the uterus typically
lies in a nearly transverse plane. The
position of the uterus changes with the degree of fullness of
the bladder and rectum, and stage of pregnancy.
Although its size varies considerably, the non-gravid uterus
is approximately 7.5 cm long, 5 cm wide, and 2 cm thick and
weighs approximately 90 g. The uterus is divisible into two
main parts: the body and cervix.
The body of the uterus, forming the superior two thirds of
the organ, includes the fundus of the uterus, the rounded part
that lies superior to the uterine ostia. The body lies
between the layers of the broad ligament and is freely movable. It has two surfaces: vesical (related to the bladder) and intestinal. The body is demarcated from the cervix by
the isthmus of the uterus, a relatively constricted segment,
approximately 1 cm long.
The cervix of the uterus is the cylindrical, relatively narrow inferior third of the uterus, approximately 2.5 cm long
in an adult non-pregnant woman. For descriptive purposes,
two parts are described: a supravaginal part between the
isthmus and the vagina, and a vaginal part, which protrudes
into the superiormost anterior vaginal wall.
The rounded vaginal part surrounds the external os of the
uterus and is surrounded in turn by a narrow recess, the vaginal fornix. The supravaginal part is separated from the bladder anteriorly by loose connective tissue
and from the rectum posteriorly by the recto-uterine pouch.
The slit-like uterine cavity is approximately 6 cm
in length from the external os to the wall of the fundus. The uterine horns (Latin cornua) are the
superolateral regions of the uterine cavity, where the
uterine tubes enter. The uterine cavity continues inferiorly as the cervical canal. The fusiform canal extends
from a narrowing inside the isthmus of the uterine body,
the anatomical internal os, through the supravaginal
and vaginal parts of the cervix, communicating with the lumen of the vagina through the external os. The uterine
cavity (in particular, the cervical canal) and the lumen of
the vagina together constitute the birth canal, through
which the fetus passes at the end of gestation.
The wall of the body of the uterus consists of three coats,
or layers:
• Perimetrium - the serosa or outer serous coat - consists of
peritoneum supported by a thin layer of connective tissue.
• Myometrium - the middle coat of smooth muscle - becomes greatly distended (more extensive but much thinner) during pregnancy. The main branches of the
blood vessels and nerves of the uterus are located in this
coat. During childbirth, contraction of the myometrium is hormonally stimulated at intervals of decreasing length
to dilate the cervical os and expel the fetus and placenta.
During the menses, myometrial contractions may produce cramping.
• Endometrium - the inner mucous coat - is firmly
adhered to the underlying myometrium. The endometrium is actively involved in the menstrual cycle, differing
in structure with each stage of the cycle. If conception
occurs, the blastocyst becomes implanted in this layer; if
conception does not occur, the inner surface of this coat
is shed during menstruation.
The amount of muscular tissue in the cervix is markedly less
than in the body of the uterus. The cervix is mostly fibrous
and is composed mainly of collagen with a small amount of
smooth muscle and elastin.
Ligaments of Uterus
Externally, the ligament of the
ovary attaches to the uterus postero-inferior to the uterotubal junction. The round ligament of the
uterus (Latin ligamentum teres uteri) attaches antero-inferiorly
to this junction. These two ligaments are vestiges of the ovarian gubernaculum, related to the relocation of the gonad
from its developmental position on the posterior abdominal
wall.
The broad ligament of the uterus is a double layer
of peritoneum (mesentery) that extends from the sides of
the uterus to the lateral walls and floor of the pelvis. This ligament assists in keeping the uterus in position. The two layers of the broad ligament are continuous
with each other at a free edge that surrounds the uterine
tube. Laterally, the peritoneum of the broad ligament is
prolonged superiorly over the vessels as the suspensory
ligament of the ovary. Between the layers of the broad ligament on each side of the uterus, the ligament of the ovary lies posterosuperiorly and the round ligament of the uterus
lies antero-inferiorly. The uterine tube lies in the anterosuperior free border of the broad ligament, within a small
mesentery called the mesosalpinx. Similarly, the ovary lies
within a small mesentery called the mesovarium on the
posterior aspect of the broad ligament. The largest part of
the broad ligament, inferior to the mesosalpinx and mesovarium, which serves as a mesentery for the uterus itself,
is the mesometrium.
The uterus is a dense structure located in the center
of the pelvic cavity. The principal supports of the uterus
holding it in this position are both passive and active or
dynamic. Dynamic support of the uterus is provided by
the pelvic diaphragm. Its tone during sitting and standing and active contraction during periods of increased intra-abdominal pressure (sneezing, coughing, etc.) is transmitted through the surrounding pelvic organs and the
endopelvic fascia in which they are embedded. Passive
support of the uterus is provided by its position - the way in which the normally anteverted and anteflexed uterus
rests on top of the bladder. When intra abdominal pressure is increased, the uterus is pressed against the bladder.
The cervix is the least mobile part of the uterus because
of the passive support provided by attached condensations
of endopelvic fascia (ligaments), which may also contain
smooth muscle:
• Cardinal (transverse cervical) ligaments extend from the
supravaginal cervix and lateral parts of the fornix of the
vagina to the lateral walls of the pelvis.
• Uterosacral ligaments pass superiorly and slightly posteriorly from the sides of the cervix to the middle of the
sacrum; they are palpable during a rectal examination.
Together these passive and active supports keep the uterus
centered in the pelvic cavity and resist the tendency for
the uterus to fall or be pushed through the vagina.
Relations of Uterus
Peritoneum covers the uterus
anteriorly and superiorly, except for the cervix.
The peritoneum is reflected anteriorly from the uterus onto
the bladder and posteriorly over the posterior part of the fornix of the vagina to the rectum. Anteriorly, the
uterine body is separated from the urinary bladder by the
vesico-uterine pouch, where the peritoneum is reflected from the uterus onto the posterior margin of the superior
surface of the bladder. Posteriorly, the uterine body and
supravaginal part of the cervix are separated from the sigmoid colon by a layer of peritoneum, and the peritoneal
cavity and from the rectum by the recto-uterine pouch. Laterally, the uterine artery crosses the ureter superiorly, near
the cervix.
Summary of the relations of the uterus:
• Anteriorly (antero-inferiorly in its normal anteverted position): the vesico-uterine pouch and superior surface of the
bladder; the supravaginal part of the cervix is related to
the bladder and is separated from it by only fibrous connective tissue.
• Posteriorly: the recto-uterine pouch containing loops of
small intestine and the anterior surface of rectum; only
the visceral pelvic fascia uniting the rectum and uterus
here resists increased intra-abdominal pressure.
• Laterally: the peritoneal broad ligament flanking the
uterine body and the fascial cardinal ligaments on each
side of the cervix and vagina; in the transition between
the two ligaments, the ureters run anteriorly slightly
superior to the lateral part of the vaginal fornix and
inferior to the uterine arteries, usually approximately
2 cm lateral to the supravaginal part of the cervix.
Arterial Supply and Venous Drainage of Uterus
The
blood supply of the uterus derives mainly from the uterine
arteries, with potential collateral supply from the ovarian
arteries. The uterine veins enter the broad ligaments with the arteries and form a uterine venous plexus
on each side of the cervix. Veins from the uterine plexus drain into the internal iliac veins.