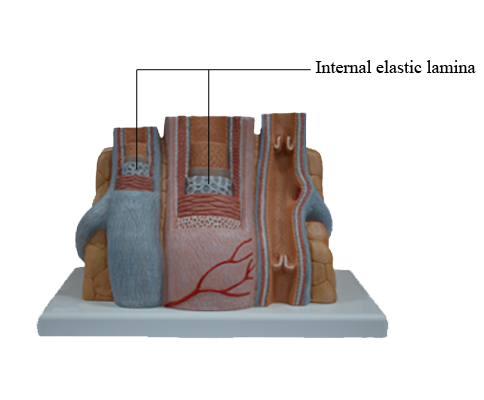
Main Model
Anterior : Internal elastic lamina
Arteries
Arteries conduct blood from the heart to the capillaries. They store some of the pumped blood during each cardiac systole to ensure continued flow through the capillaries during cardiac diastole.
Arteries are organized in three major tunics or layers:
1. The tunica intima is the innermost coat. It consists of an endothelial lining continuous with the endocardium, the inner lining of the heart; an intermediate layer of loose connective tissue, the subendothelium; and an external layer of elastic fibers, the internal elastic lamina.
2. The tunica media is the middle coat. It consists mainly of smooth muscle cells surrounded by a variable number of collagen fibers, extracellular matrix, and elastic sheaths with irregular gaps (fenestrated elastic membranes).
Collagen fibers provide a supporting framework for smooth muscle cells and limit the distensibility of the wall of the vessel. Veins have a higher content of collagen than arteries.
3. The tunica externa, or adventitia, is the outer coat and consists mainly of connective tissue. An external elastic lamina can be seen separating the tunica media from the adventitia.
The adventitia of large vessels (arteries and veins) contains small vessels (vasa vasorum) that penetrate the outer portion of the tunica media to supply oxygen and nutrients.
From the heart to the capillaries, arteries can be classified into three major groups:
1. Large-sized elastic arteries.
2. Medium-sized muscular arteries.
3. Small-sized arteries and arterioles.
Large elastic arteries are conducting vessels
The aorta and its largest branches (the brachiocephalic, common carotid, subclavian, and common iliac arteries) are elastic arteries. They are conducting arteries because they conduct blood from the heart to the medium-sized distributing arteries.
Large elastic arteries have two major characteristics:
1. They receive blood from the heart under high pressure.
2. They keep blood circulating continuously while the heart is pumping intermittently.
Because they distend during systole and recoil during diastole, elastic arteries can sustain a continuous blood flow despite the intermittent pumping action of the heart.
The tunica intima of the elastic arteries consists of the endothelium and the subendothelial connective tissue.
Large amounts of fenestrated elastic sheaths are found in the tunica media, with bundles of smooth muscle cells permeating the narrow gaps between the elastic lamellae. Collagen fibers are present in all tunics, but especially in the adventitia. The smooth muscle cells can synthesize both elastic and collagen fibers. Blood vessels (vasa vasorum), nerves (nervi vasorum), and lymphatics can be recognized in the tunica adventitia of large elastic arteries.
Pathology: Aortic aneurysms
Aneurysms are dilatations of arteries; the dilatations of veins are called varices.
The two major types of aortic aneurysms are the syphilitic aneurysm (relatively rare because syphilis is no longer common) and the abdominal aneurysm.
Syphilitic aneurysms are mostly localized in the ascending aorta and its arch. Abdominal aneurysms are caused by a weakening of the aortic wall produced by atherosclerosis.
Aortic aneurysms generate murmurs caused by blood turbulence in the dilated aortic segment. A severe complication of an aneurysm is aortic dissection caused by a tear in the tunica intima that enables blood to penetrate and form an intramural hematoma between the intima and the tunica media or the media and the tunica adventitia. Aortic dissection is associated with high mortality caused by exsanguination.
Marfan syndrome is an autosomal dominant defect associated with aortic dissecting aneurysm and skeletal and ocular abnormalities due to mutations in the fibrillin 1 gene. Fibrillins are major components of the elastic fibers found in the aorta, periosteum, and suspensory ligament of the lens.
Medium-sized muscular arteries are distributing vessels
There is a gradual transition from large arteries, to medium-sized arteries, to small arteries and arterioles. Medium-sized arteries are distributing vessels, allowing a selective distribution of blood to different organs in response to functional needs. Examples of medium-sized arteries include the radial, tibial, popliteal, axillary, splenic, mesenteric, and intercostal arteries. The diameter of medium-sized muscular arteries is about 3 mm or greater.
The tunica intima consists of three layers:
1. The endothelium.
2. The subendothelium.
3. The internal elastic lamina.
The internal elastic lamina is a fenestrated band of elastic fibers that often shows folds in sections of fixed tissue because of contraction of the smooth muscle cell layer (tunica media).
The tunica media shows a significant reduction in elastic components and an increase in smooth muscle fibers. In the larger vessels of this group, a fenestrated external elastic lamina can be seen at the junction of the tunica media and the adventitia.
Arterioles are resistance vessels
Arterioles are the final branches of the arterial system. Arterioles regulate the distribution of blood to different capillary beds by vasoconstriction and vasodilation in localized regions. Partial contraction (known as tone) of the vascular smooth muscle exists in arterioles. Arterioles are structurally adapted for vasoconstriction and vasodilation because their walls contain circularly arranged smooth muscle fibers. Arterioles are regarded as resistance vessels and are the major determinants of systemic blood pressure.
The diameter of arterioles and small arteries ranges from 20 to 130 micrometer. Because the lumen is small, these blood vessels can be closed down to generate high resistance to blood flow.
The tunica intima has an endothelium, subendothelium, and internal elastic lamina. The tunica media consists of two to five concentric layers of smooth muscle cells. The tunica adventitia, or tunica externa, contains slight collagenous tissue, binding the vessel to its surroundings.
The segment beyond the arteriole proper is the metarteriole, the terminal branch of the arterial system. It consists of one layer of muscle cells, often discontinuous, and represents an important local regulator of blood flow.
Capillaries are exchange vessels
Capillaries are extremely thin tubes formed by a single layer of highly permeable endothelial cells surrounded by a basal lamina. The diameter range of a capillary is about 5 to 10 micrometer, large enough to accommodate one red blood cell, and thin enough (0.5 micrometer) for gas diffusion.
The microvascular bed, the site of the microcirculation, is composed of the terminal arteriole (and metarteriole), the capillary bed, and the postcapillary venules. The capillary bed consists of slightly large capillaries (called preferential or thoroughfare channels), where blood flow is continuous, and small capillaries, called the true capillaries, where blood flow is intermittent.
The amount of blood entering the microvascular bed is regulated by the contraction of smooth muscle fibers of the precapillary sphincters located where true capillaries arise from the arteriole or metarteriole. The capillary circulation can be bypassed by channels (through channels) connecting terminal arterioles to postcapillary venules.
When functional demands decrease, most precapillary sphincters are closed, forcing the flow of blood into thoroughfare channels. Arteriovenous shunts, or anastomoses, are direct connections between arterioles and postcapillary venules and bypass the microvascular bed.
The three-dimensional design of the microvasculature varies from organ to organ. The local conditions of the tissues (concentration of nutrients and metabolites and other substances) can control local blood flow in small portions of a tissue area.
Types of Capillaries
Three morphologic types of capillaries are recognized:
1. Continuous.
2. Fenestrated.
3. Discontinuous (sinusoids).
Continuous capillaries are lined by a complete simple squamous endothelium and a basal lamina. Pericytes can occur between the endothelium and the basal lamina. Pericytes are undifferentiated cells that resemble modified smooth muscle cells and are distributed at random intervals in close contact with the basal lamina. Endothelial cells are linked by tight junctions and transport fluids and solutes by caveolae and pinocytotic vesicles. Continuous capillaries occur in the brain, muscle, skin, thymus, and lungs.
Fenestrated capillaries have pores, or fenestrae, with or without diaphragms. Fenestrated capillaries with a diaphragm are found in intestines, endocrine glands, and around kidney tubules. Fenestrated capillaries without a diaphragm are characteristic of the renal glomerulus. In this particular case, the basal lamina constitutes an important permeability barrier.
Discontinuous capillaries are characterized by an incomplete endothelial lining and basal lamina, with gaps or holes between and within endothelial cells. Discontinuous capillaries and sinusoids are found where an intimate relation is needed between blood and parenchyma (for example, in the liver and spleen).
Veins are capacitance, or reservoir, vessels
The venous system starts at the end of the capillary bed with a postcapillary venule that structurally resembles continuous capillaries but with a wider lumen.
Postcapillary venules, the preferred site of migration of blood cells into tissues by a mechanism called diapedesis (Greek dia, through; pedan, to leap), are tubes of endothelial cells supported by a basal lamina and an adventitia of collagen fibers and fibroblasts.
In lymphatic tissues, the endothelial cells are taller. High endothelial venules are associated with the mechanism of homing of lymphocytes in lymphoid organs.
Postcapillary venules converge to form muscular venules, which converge into collecting venules, leading to a series of veins of progressively larger diameter.
Veins have a relatively thin wall in comparison with arteries of the same size. The high capacitance of veins is attributable to the distensibility of their wall (compliance vessels) and, therefore, the content of blood is large relative to the volume of the veins. A small increase in the intraluminal pressure results in a large increase in the volume of contained blood.
Similar to arteries, veins consist of tunics. However, the distinction of a tunica media from a tunica adventitia is often not clear. The lumen is lined by an endothelium and a subjacent basal lamina. A distinct internal elastic lamina is not seen.
The muscular tunica media is thinner than in arteries, and smooth muscle cells have an irregular orientation, approximately circular. A longitudinal orientation is observed in the iliac vein, brachiocephalic vein, superior and inferior venae cavae, portal vein, and renal vein.
The tunica adventitia consists of collagen fibers and fibroblasts with few nerve fibers. In large veins, the vasa vasorum penetrate the wall.
A typical characteristic of veins is the presence of valves to prevent reflux of blood. A valve is a projection into the lumen of the tunica intima, covered by endothelial cells and strengthened by elastic and collagen fibers.
Examples of varices (dilatations of veins) are hemorrhoids (varices of the internal or external plexus of the rectum), varicocele (varices of the pampiniform plexus of the spermatic cord), varicose veins of the legs and varices of the esophagus (associated with portal hypertension and cirrhosis of the liver).
Pathology: Vasculitis
Vasculitis defines the acute and chronic inflammation of vessels. It can be caused by infectious and immunologic pathogens. Bacterial and rickettsial infection, syphilis and fungi cause vasculitis, thrombophlebitis (thrombosis and inflammation of the wall of a vein) and pseudoaneurysms (dilation of the wall of a blood vessel by the lytic activity of bacterial enzymes.
Most inflammatory conditions of the wall of arteries involve an immune-based pathogenesis.
Antigen-antibody complexes, accumulating in the wall of a blood vessel, can activate the complement cascade. When neutrophils are attracted by chemotactic fragments released by the activated complement cascade and exposed to cytokines, they release serine proteinase 3 and myeloperoxidase, capable of causing damage to the vascular wall.
Antibodies reacting with cytoplasmic components of neutrophils (anti-neutrophil cytoplasmic antibody, ANCA) release enzymes from the activated neutrophils, causing vascular wall injury.
Serine proteinase 3, a component of cytoplasmic granules in neutrophils, is the antigen that generates C-ANCA (cytoplasmic ANCA); P-ANCA are antibodies to myeloperoxidase showing a perinuclear pattern in neutrophils (perinuclear ANCA) by immunocytochemistry.
Vasculitis include:
1. Giant cell arteritis is a common form of vasculitis in adults (over the age of 50) that affects temporal, ophthalmic or vertebral arteries. Headache, pain in the shoulders, hips and jaw claudication as well as an elevated erythrocyte sedimentation rate are common findings. Blindness from giant cell arteritis of the ophthalmic artery is irreversible if the disease is not treated early with prednisone. A biopsy of the temporal artery, showing in most cases giant multinucleated cells (macrophages) and lymphocyte infiltrates in the wall, thickening of the tunica intima and thrombosis, confirms the nature of the disease.
2. Buerger's disease (thromboangitis obliterans), involves medium-sized and small arteries of hands and feet of young males who are heavy cigarette smokers. Typical symptoms are claudication, pain in hands and feet caused by insufficient blood flow during exercise, and Raynaud's phenomenon, a condition in which fingers and toes turn white upon exposure to cold. Angiograms of the upper and lower extremities generally show blockage or narrowing segments. Stopping smoking is the most effective treatment.
3. Polyarteritis nodosa (PAN) affects the wall of medium- to small-sized arteries of the skin, kidneys, liver, heart, and gastrointestinal tract. PAN has been associated with active hepatitis B and/or hepatitis C. The disease is more common in injection drug users. Immune complexes (immunoglobulin and viral antigens) circulating in the blood accumulate in the vascular wall. Prednisone is the effective treatment of PAN.
4. Giant cell aortitis (Takayasu's arteritis) is a rare disease that occurs with a high frequency in Asian women under the age of 40 and affects the aorta and its branches. It consists of an inflammatory phase followed by an occlusive phase, the narrowing and segmental dilation of the aorta and/or its branches, resulting in absent pulses. Takayasu's arteritis and giant cell arteritis are histologically similar: both show destruction of the blood vessel wall and giant multinucleated cells.
5. Kaswasaki's disease affects the coronary arteries as well as large, medium- and small-sized arteries of children. It is associated with fever, ulcerations of mouth, lips and throat mucosae and lymph node enlargement. The standard treatment includes intravenous immunoglobulin and aspirin. Affected children recover without serious complications.
6. Churg-Strauss syndrome (CSS) is a systemic vasculitis associated with asthma, rhinitis and eosinophilia. A biopsy of an affected blood vessel shows perivascular eosinophils. The cause of CSS is unknown.
7. Wegener's granulomatosis is a necrotizing arteritis of the respiratory tract and kidneys. Although C-ANCAs are frequently present in patients with Wegener's granulomatosis, a lung biopsy is the most effective way of diagnosing this condition. The wall of blood vessels shows vasculitis, granulomas and extensive necrosis.
8. Henoch-Schönlein purpura (HSP) is the most common form of vasculitis in children. It is associated with purpura (purple-colored spots of the skin and mucosae), arthritis, nephritis and abdominal pain. In most cases, HSP follows upper respiratory tract infections. A typical finding in skin biopsies is the deposition of immunoglobulin A in the walls of affected blood vessels. HSP frequently resolves in a few weeks.