Main Model
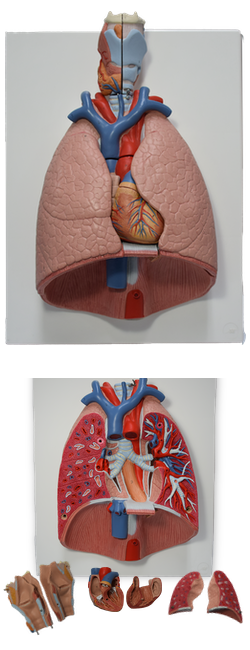
G DIAPHRAGM
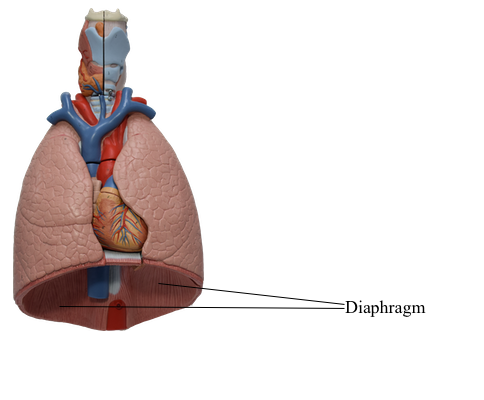
Diaphragm
The diaphragm is a double-domed, musculotendinous
partition separating the thoracic and abdominal cavities. Its
mainly convex superior surface faces the thoracic cavity, and
its concave inferior surface faces the abdominal cavity. The diaphragm is the chief muscle of inspiration (actually, of respiration altogether, because expiration
is largely passive). It descends during inspiration; however,
only its central part moves because its periphery, as the fixed
origin of the muscle, attaches to the inferior margin of the
thoracic cage and the superior lumbar vertebrae.
The pericardium, containing the heart, lies on the central
part of the diaphragm, depressing it slightly. The
diaphragm curves superiorly into right and left domes; normally the right dome is higher than the left dome owing to
the presence of the liver. During expiration, the right dome reaches as high as the 5th rib and the left dome ascends to
the 5th intercostal space. The level of the domes of the diaphragm varies according to the:
• Phase of respiration (inspiration or expiration).
• Posture (e.g., supine or standing).
• Size and degree of distension of the abdominal viscera.
The muscular part of the diaphragm is situated peripherally with fibers that converge radially on the trifoliate central
aponeurotic part, the central tendon. The
central tendon has no bony attachments and is incompletely divided into three leaves, resembling a wide cloverleaf. Although it lies near the center of the diaphragm,
the central tendon is closer to the anterior part of the thorax.
The caval opening (vena caval foramen), through which
the terminal part of the IVC passes to enter the heart, perforates the central tendon. The surrounding muscular part
of the diaphragm forms a continuous sheet; however, for
descriptive purposes it is divided into three parts, based on
the peripheral attachments:
• Sternal part: consisting of two muscular slips that attach
to the posterior aspect of the xiphoid process; this part is
not always present.
• Costal part: consisting of wide muscular slips that attach
to the internal surfaces of the inferior six costal cartilages
and their adjoining ribs on each side; the costal parts form
the right and left domes.
• Lumbar part: arising from two aponeurotic arches, the
medial and lateral arcuate ligaments, and the three superior lumbar vertebrae; the lumbar part forms right and left
muscular crura that ascend to the central tendon.
The crura of the diaphragm are musculotendinous bands
that arise from the anterior surfaces of the bodies of the
superior three lumbar vertebrae, the anterior longitudinal
ligament, and the IV discs. The right crus, larger and longer
than the left crus, arises from the first three or four lumbar
vertebrae. The left crus arises from the first two or three
lumbar vertebrae. Because it lies to the left of the midline, it
is surprising to find that the esophageal hiatus is a formation in the right crus; however, if the muscular fibers bounding
each side of the hiatus are traced inferiorly, it will be seen
that they pass to the right of the aortic hiatus.
The right and left crura and the fibrous median arcuate ligament, which unites them as it arches over the anterior aspect of
the aorta, form the aortic hiatus. The diaphragm is also attached
on each side to the medial and lateral arcuate ligaments. The
medial arcuate ligament is a thickening of the fascia covering
the psoas major, spanning between the lumbar vertebral bodies
and the tip of the transverse process of L1. The lateral arcuate
ligament covers the quadratus lumborum muscles, continuing
from the L12 transverse process to the tip of the 12th rib.
The superior aspect of the central tendon of the diaphragm
is fused with the inferior surface of the fibrous pericardium,
the strong, external part of the fibroserous pericardial sac
that encloses the heart.
Vessels and Nerves of Diaphragm
The arteries of the diaphragm form a branch-like pattern on
both its superior (thoracic) and inferior (abdominal) surfaces.
The arteries supplying the superior surface of the diaphragm are the pericardiacophrenic and musculophrenic arteries, branches of the internal thoracic artery, and the superior phrenic arteries, arising from the thoracic aorta. The arteries supplying the inferior surface of the
diaphragm are the inferior phrenic arteries, which typically are the first branches of the abdominal aorta; however,
they may arise from the celiac trunk.
The veins draining the superior surface of the diaphragm
are the pericardiacophrenic and musculophrenic veins,
which empty into the internal thoracic veins and, on the right
side, a superior phrenic vein, which drains into the IVC.
Some veins from the posterior curvature of the diaphragm
drain into the azygos and hemi-azygos veins.
The veins draining the inferior surface of the diaphragm are
the inferior phrenic veins. The right inferior phrenic vein
usually opens into the IVC, whereas the left inferior phrenic
vein is usually double, with one branch passing anterior to
the esophageal hiatus to end in the IVC and the other, more
posterior branch usually joining the left suprarenal vein. The
right and left phrenic veins may anastomose with each other.
The lymphatic plexuses on the superior and inferior surfaces of the diaphragm communicate freely. The
anterior and posterior diaphragmatic lymph nodes are
on the superior surface of the diaphragm. Lymph from these
nodes drains into the parasternal, posterior mediastinal, and phrenic lymph nodes. Lymphatic vessels from the inferior
surface of the diaphragm drain into the anterior diaphragmatic, phrenic, and superior lumbar (caval/aortic) lymph
nodes. Lymphatic capillaries are dense on the inferior surface of the diaphragm, constituting the primary means for
absorption of peritoneal fluid and substances introduced by
intraperitoneal (I.P.) injection.
The entire motor supply to the diaphragm is from the
right and left phrenic nerves, each of which arises from the
anterior rami of C3-C5 segments of the spinal cord and is
distributed to the ipsilateral half of the diaphragm from its inferior surface. Sensory innervation (pain and proprioception) to the diaphragm is also mostly from the
phrenic nerves. Peripheral parts of the diaphragm receive
their sensory nerve supply from the intercostal nerves (lower
six or seven) and the subcostal nerves.
Diaphragmatic Apertures
The diaphragmatic apertures (openings, hiatus) permit
structures (vessels, nerves, and lymphatics) to pass between
the thorax and abdomen. There
are three large apertures for the IVC, esophagus, and aorta
and a number of small ones.
Caval Opening
The caval opening is an aperture in the central tendon primarily for the IVC. Also passing through the caval opening
are terminal branches of the right phrenic nerve and a few
lymphatic vessels on their way from the liver to the middle
phrenic and mediastinal lymph nodes. The caval opening is
located to the right of the median plane at the junction of the
central tendon's right and middle leaves. The most superior
of the three large diaphragmatic apertures, the caval opening
lies at the level of the IV disc between the T8 and T9 vertebrae. The IVC is adherent to the margin of the opening; consequently, when the diaphragm contracts during inspiration, it widens the opening and dilates the IVC. These changes
facilitate blood flow through this large vein to the heart.
Esophageal Hiatus
The esophageal hiatus is an oval opening for the esophagus in the muscle of the right crus of the diaphragm at the
level of the T10 vertebra. The esophageal hiatus also transmits
the anterior and posterior vagal trunks, esophageal branches
of the left gastric vessels, and a few lymphatic vessels. The
fibers of the right crus of the diaphragm decussate (cross one
another) inferior to the hiatus, forming a muscular sphincter
for the esophagus that constricts it when the diaphragm contracts. The esophageal hiatus is superior to and to the left of
the aortic hiatus. In most individuals (70%), both margins of
the hiatus are formed by muscular bundles of the right crus. In
others (30%), a superficial muscular bundle from the left crus
contributes to the formation of the right margin of the hiatus.
Aortic Hiatus
The aortic hiatus is the opening posterior in the diaphragm
for the descending aorta. Because the aorta does not pierce the
diaphragm, movements of the diaphragm do not affect blood
flow through the aorta during respiration. The aorta passes
between the crura of the diaphragm posterior to the median
arcuate ligament, which is at the level of the inferior border of
the T12 vertebra. The aortic hiatus also transmits the thoracic
duct and sometimes the azygos and hemi-azygos veins.
Small Openings in Diaphragm
In addition to the three main apertures, there is a small opening, the sternocostal triangle (foramen), between the sternal and costal attachments of the diaphragm. This triangle transmits lymphatic vessels from the diaphragmatic surface of
the liver and the superior epigastric vessels. The sympathetic
trunks pass deep to the medial arcuate ligament, accompanied by the least splanchnic nerves. There are two small apertures in each crus of the diaphragm; one transmits the greater
splanchnic nerve and the other the lesser splanchnic nerve.
Actions of Diaphragm
When the diaphragm contracts, its domes are pulled inferiorly
so that the convexity of the diaphragm is somewhat flattened.
Although this movement is often described as the "descent of
the diaphragm," only the domes of the diaphragm descend.
The diaphragm's periphery remains attached to the ribs and
cartilages of the inferior six ribs. As the diaphragm descends, it pushes the abdominal viscera inferiorly. This increases the
volume of the thoracic cavity and decreases the intrathoracic
pressure, resulting in air being taken into the lungs. In addition, the volume of the abdominal cavity decreases slightly
and intra-abdominal pressure increases somewhat.
Movements of the diaphragm are also important in circulation
because the increased intra-abdominal pressure and decreased
intrathoracic pressure help return venous blood to the heart.
When the diaphragm contracts, compressing the abdominal viscera, blood in the IVC is forced superiorly into the heart.
The diaphragm is at its most superior level when a person
is supine (with the upper body lowered, the Trendelenburg
position). In this position, the abdominal viscera push the diaphragm superiorly in the thoracic cavity. When a person
lies on one side, the hemidiaphragm rises to a more superior
level because of the greater push of the viscera on that side.
Conversely, the diaphragm assumes an inferior level when
a person is sitting or standing. For this reason, people with
dyspnea (difficult breathing) prefer to sit up, not lie down;
non-tidal (reserve) lung volume is increased, and the diaphragm is working with gravity rather than opposing it.