Main Model

Jejunum (small intestine) : Outer mucous tissue
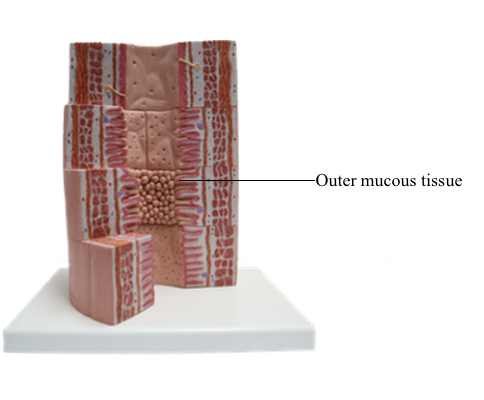
Small Intestine
The 4- to 7-meter-long small intestine is divided into
three sequential segments:
1. Duodenum.
2. Jejunum.
3. Ileum.
The duodenum is about 25 cm in length, is
mainly retroperitoneal, and surrounds the head of the pancreas. At its distal end, the duodenum is
continuous with the jejunum, a movable intestinal
segment suspended by a mesentery. The ileum is the
continuation of the jejunum.
The wall of the small intestine consists of four
layers:
1. The mucosa.
2. The submucosa.
3. The muscularis.
4. The serosa, or peritoneum.
Histologic differences are seen in
the mucosa and submucosa of the three major portions of the small intestine. The muscularis externa
and serosa layers are similar.
The Peritoneum
The peritoneum is a serous membrane consisting of
a connective tissue stroma (containing elastic fibers,
blood and lymphatic vessels, and nerves) lined by
mesothelial cells. The parietal peritoneum lines the
abdominal wall and reflects to cover the abdominal
viscera as the visceral peritoneum.
The mesentery is a layer of loose connective tissue
(areolar connective tissue) covered with peritoneum. The mesentery attaches the
abdominal viscera to the posterior abdominal wall
and it serves as a conduit of blood and lymphatic vessels and nerves to these organs. The blood vessels are
components of the subserosal plexus. During digestion, the lymphatic vessels emerging
from the walls of the small intestine carry a fluid rich
in absorbed fat emulsion, or chyle. Numerous lymph
nodes and adipose tissue are seen in the mesentery.
The mesentery can be short to anchor certain viscera
to the abdominal wall, or longer to enable visceral displacement. As indicated, the esophagus lacks a serosa. The
duodenum and ascending and descending colon attach to the abdominal cavity by the adventitia, a loose
connective tissue continuous with the surrounding
stroma of the abdominal wall.
The omenta and visceral ligaments have a structure
similar to the mesentery. The greater omentum has
considerable adipose tissue.
Intestinal Wall
The intestinal wall shows an increase in the total
surface of the mucosa that reflects the absorptive
function of the small intestine.
Four degrees of folding amplify the absorptive
surface area of the mucosa:
1. The plicae circulares (circular folds; also known
as the valves of Kerkring).
2. The intestinal villi.
3. The intestinal glands.
4. The microvilli on the apical surface of the lining
epithelium of the intestinal cells (enterocytes).
A plica circularis is a permanent fold of the mucosa
and submucosa encircling the intestinal lumen.
Plicae appear about 5 cm distal to the pyloric outlet
of the stomach, become distinct where the duodenum joins the jejunum, and diminish in size progressively
to disappear halfway along the ileum.
The intestinal villi are finger-like projections of
the mucosa covering the entire surface of the small
intestine. Villi extend deep into the mucosa to form
crypts ending at the muscularis mucosae. The length of the villi depends on the degree of distention of the
intestinal wall and the contraction of smooth muscle
fibers in the villus core.
Crypts of Lieberkühn, or intestinal glands, are
simple tubular glands that increase the intestinal surface area. The crypts are formed by invaginations
of the mucosa between adjacent intestinal villi.
The muscularis mucosae is the boundary between
the mucosa and submucosa.
The muscularis consists of inner circular smooth
muscle and outer longitudinal smooth muscle. The
muscularis is responsible for segmentation and
peristaltic movement of the contents of the small
intestine.
A thin layer of loose connective tissue is covered
by the visceral peritoneum, a serosa layer lined by a simple squamous epithelium, or mesothelium. The
parietal peritoneum covers the inner surface of the
abdominal wall.
Histologic Differences Between the Duodenum, Jejunum, and Ileum
Each of the three major anatomic portions of the
small intestine, the duodenum, jejunum, and ileum,
has distinctive features that allow recognition under
the light microscope.
The duodenum extends from the pyloric region of
the stomach to the junction with the jejunum and
has the following characteristics:
1. It has Brunner's glands in the submucosa.
Brunner's glands are tubuloacinar mucous glands producing an alkaline secretion (pH 8.8 to 9.3)
that neutralizes the acidic chyme coming from the
stomach.
2. The villi are broad and short (leaflike shape).
3. The duodenum is surrounded by an incomplete
serosa and an extensive adventitia rather than a serosa.
4. The duodenum collects bile and pancreatic
secretions transported by the common bile duct and
pancreatic duct, respectively. The sphincter of Oddi
is present at the terminal ampullary portion of the
two converging ducts.
5. The base of the crypts of Lieberkühn may contain Paneth cells.
The jejunum has the following characteristics:
1. It has long finger-like villi and a well-developed
lacteal in the core of the villus.
2. The jejunum does not contain Brunner's glands
in the submucosa.
3. Peyer's patches in the lamina propria may be
present but they are not predominant in the jejunum.
Peyer's patches are a characteristic feature of the ileum.
4. Paneth cells are found at the base of the crypts
of Lieberkühn.
The ileum has a prominent diagnostic feature:
Peyer's patches, lymphoid follicles (also called nodules) found in the mucosa and part of the submucosa. The lack of Brunner's glands and the presence
of shorter finger-like villi, when compared with the
jejunum, are additional landmarks of the ileum. As
in the jejunum, Paneth cells are found at the base of
the crypts of Lieberkühn.
Villi and Crypts of Lieberkühn
The intestinal mucosa, including the crypts of Lieberkühn, are lined by a simple columnar epithelium
containing five major cell types:
1. Enterocytes or absorptive cells.
2. Goblet cells.
3. Enteroendocrine cells.
4. Paneth cells.
5. Intestinal stem cells.
Enteroendocrine cells, Paneth cells, and intestinal
stem cells are found in the crypts of Lieberkühn.
Enterocytes: Absorptive Cells
The absorptive intestinal cell or enterocyte has an
apical domain with a prominent brush border (also
called a striated border), ending on a zone, called the
terminal web, which contains transverse cytoskeletal
filaments. The brush border of each absorptive cell
contains about 3000 closely packed microvilli, which
increase the surface luminal area 30-fold.
The length of a microvillus ranges from 0.5 to 1.0micrometer. The core of a microvillus contains
a bundle of 20 to 40 parallel actin filaments cross-linked by fimbrin and villin. The actin bundle core
is anchored to the plasma membrane by formin (protein of the cap), myosin I, and the calcium-binding
protein calmodulin. Each actin bundle projects into
the apical portion of the cell as a rootlet, which is cross-linked by an intestinal isoform of spectrin to
an adjacent rootlet. The end portion of the rootlet
attaches to cytokeratin-containing intermediate filaments. Spectrin and cytokeratins form part of the
terminal web. The terminal web is responsible for
maintaining the upright position and shape of the
microvillus and anchoring the actin rootlets.
A surface coat or glycocalyx, consisting of glycoproteins as integral components of the plasma membrane, covers each microvillus.
Goblet Cells
Goblet cells are columnar mucus-secreting cells scattered among enterocytes of the intestinal epithelium.
Goblet cells have two domains:
1. A cup- or goblet-shaped apical domain containing large mucus granules that are discharged on the
surface of the epithelium.
2. A narrow basal domain, which attaches to the
basal lamina. The basal domain houses the rough
endoplasmic reticulum and Golgi apparatus, in
which the protein portion of mucus is produced and
transported, and the nucleus.
The Golgi apparatus, which adds oligosaccharide
groups to mucus, is prominent and situated above
the basally located nucleus.
The secretory product of goblet cells contains
glycoproteins (80% carbohydrate and 20% protein)
released by exocytosis.
On the surface of the epithelium, the mucus hydrates to form a protective gel coat to shield the epithelium from mechanical abrasion and bacterial
invasion by concentrating specific antimicrobial proteins, including defensins and cathelicidins.
Enteroendocrine Cells
In addition to its digestive function, the gastrointestinal tract is the largest diffuse endocrine gland
in the body.
As in the stomach, enteroendocrine cells secrete peptide
hormones controlling several functions of the gastrointestinal system.
Intestinal Stem Cells
Intestinal stem cells (ISCs) reside in a niche at the
base of the crypts, close to Paneth cells.
Adult ISC, identified by the protein marker Lgr5
(for leucine-rich repeat-containing G protein coupled receptor 5), can differentiate into the secretory
goblet cells, Paneth cells, and enteroendocrine cells
and the absorptive enterocytes lining the epithelium
of the small intestine.
ISCs are multipotent and capable of long-term
self-renewal as long as they remain at the crypt niche. Presumably ISCs are subject to positional cues
derived from the microenvironment of the niche.
As clusters of enterocytes and goblet cells divide
and differentiate, they migrate along the walls of the
crypts and villi until they reach the tip of the villus
where they are eventually shed.
Following injury, cells committed to the intestinal secretory pathway and expressing Delta-like 1
(DLL1), a ligand of the Notch family of proteins,
can return to the stem cell compartment and revert
into multipotent ISCs.
Protection of the Small Intestine
The large surface area of the gastrointestinal tract,
about 200 m2 in humans, is vulnerable to resident
microorganisms, called microbiota, and potentially
harmful microorganisms and dietary antigens. Microbiota includes bacteria, fungi, parasites and viruses.
In the small and large intestines, goblet cells secrete
mucin glycoproteins assembled into a viscous gel-like
blanket limiting direct bacterial contact with enterocytes. When the blanket lacks one of its components,
mucin glycoprotein 2 (MIC2), spontaneous intestinal
inflammation occurs.
Several defensive mechanisms operate in the alimentary tube to limit tissue invasion of pathogens and avoid potentially harmful overreactions that could
damage intestinal tissues. The defensive mechanisms
include:
1. The intestinal tight junction barrier, formed by
apical tight junctions linking enterocytes. The barrier
of pathogens is monitored by the immune-competent cells residing in the subjacent lamina propria.
2. Peyer's patches and associated M cells, regarded
as the immune sensors of the small intestine.
3. Polymeric immunoglobulin A (IgA), a secretory
product of plasma cells located in the lamina propria,
reaching the intestinal lumen by the mechanism of
transcytosis.
4. Paneth cells, whose bacteriostatic secretions
control the resident microbiota of the small intestine.
In addition, it is to be kept in mind the defensive
roles of the acidity of the gastric juice, that inactivates ingested microorganism, and the propulsive
intestinal motility (peristalsis), that prevents bacterial colonization.
Intestinal Tight Junction Barrier
Intestinal tight junctions link adjacent enterocytes
and provide a barrier function impermeable to most
hydrophilic solutes in absence of specific transporters.
Tight junctions establish a separation between the intestinal luminal content and the mucosal immune function that occurs within the lamina
propria. Plasma cells, lymphocytes, eosinophils, mast
cells and macrophages are present in the intestinal
lamina propria.
Claudin and occludin are two transmembrane
proteins of tight junctions that regulate solute permeability of the transcellular pathway. Flux of dietary
proteins and bacterial lipopolysaccharides across
leaky tight junctions can increase in the presence
of tumor necrosis factor ligand and interferon-a,
two proinflammatory cytokines that affect tight
junction integrity.
Many diseases associated with intestinal epithelial
dysfunction, including inflammatory bowel disease
and intestinal ischemia, are associated with increased
levels of tumor necrosis factor ligand.
A minor defect of the tight junction barrier can allow bacterial products or dietary antigens to cross the
epithelium and enter the lamina propria. Antigens
can bind to Toll-like receptor (TLR) on the surface
of dendritic cells.
Dendritic cells migrate to a local mesentery lymph
node and the antigen is presented to naïve T cells by
the major histocompatibility complex to determine
their differentiation into T helper 1 (TH1) and T helper 2 (TH2) cells that relocate to the lamina
propria.
TH1 cells produce the proinflammatory cytokines
tumor necrosis factor ligand and interferon-gamma. TH2
cells downregulate the proinflammatory activity of
TH1 cells by secreting interleukin-10. If the mucosa immune cell activation response proceeds unchecked, proinflammatory cytokines will continue
enhancing further leakage across the tight junction barrier, a condition leading to intestinal chronic
inflammatory diseases.
Peyer's Patches
Peyer's patches, the main component of the gut-associated lymphoid tissue (GALT), are specialized
lymphoid follicles found predominantly in the intestinal mucosa and part of the submucosa of the ileum. GALTs participate in the uptake of
antigens and their exposure to antigen-presenting
cells. Therefore, these structures serve important
functions that can lead to inflammation or tolerance.
The microbiota is involved in the normal development and maturation of GALTs. In the fetus, lymphoid tissue inducer cells stimulate the development
of Peyer's patches in the absence of microbiota.
Peyer's patches consist of cells able to take up and
transport luminal antigens and bacteria to antigen-presenting cells leading to immune tolerance or an
inflammatory reaction against pathogens.
Peyer's patches are regarded the immune sensors of
the small intestine. An equivalent to Peyer's patches
in the large intestine are the isolated lymphoid follicles (ILFs), requiring TLRs and nucleotide-binding
oligomerization domain 2 (NOD2) to become activated. TLRs are extracellular sensors and NODs are
cytoplasmic sensors.
A Peyer's patch displays three main components:
1. The follicle-associated epithelium (FAE), consisting of M cells and enterocytes.
2. The lymphoid follicles, each showing a germinal
center and a subepithelial dome area.
3. The interfollicular area, with blood vessels and
efferent lymphatic vessels connecting Peyer's patches
to the mesenteric lymph nodes.
High endothelial venules, enabling the immigration of lymphocytes, are present in the lymphoid follicles. Activated lymphocytes leave the Peyer's patches
through the lymphatic vessels.
The main components of the FAE are M cells and
dendritic cells:
1. M cells, forming an enterocyte specialized cell layer that takes up antigens
and replaced the brush border by short microfolds
(hence the name M cell). M cells differentiate from enterocytes when stimulated by membrane-bound
lymphotoxin (LT_1`2) present on local B cells.
M cells form intraepithelial pockets, where a subpopulation of intraepithelial B cells resides and express
IgA receptors allowing the capture and phagocytosis
of IgA-bound bacteria.
Antigens are transported by M cell and presented to the immunocompetent B cells residing in the
intraepithelial pockets.
The population of M cells increases rapidly in the
presence of pathogenic bacteria in the intestinal lumen (for example, Salmonella typhimurium). When
confronting Salmonella, the microfolds of M cells
change into large ruffles and, within 30 to 60 minutes, M cells undergo necrosis and the population
of M cells is depleted. Poliovirus, the pathogen of
poliomyelitis, uses the Peyer's patches to replicate.
2. Dendritic cell, extending cytoplasmic processes
between tight junctions linking enterocytes.
Lymphoid follicles have a germinal center that
contains IgA-positive B cells, CD4+ T cells, antigen-presenting cells and follicular dendritic cells. A few
plasma cells are present in the Peyer's patches. The
subepithelial dome contains B cells, T cells, macrophages, and dendritic cells.
Antigens in the intestinal lumen activate TLRs expressed by enterocytes. TLR-antigen interaction stimulates the production of B
cell-activating factor (BAF) and cytokines to activate the production of immunoglobulin (Ig) A by plasma
cells located in the lamina propria and Peyer's patches.
Intestinal antigens, bound to immunoglobulin
receptors on the surface of B cells, interact with antigen-presenting cells at the subepithelial dome
region. Antigens are presented to follicular dendritic
cells and CD4+ T cells to initiate an immune reaction.
In summary, Peyer's patches have the ability to
transport luminal antigens and microorganisms and
respond to them by inducing immune tolerance or
a systemic immune defense response. An example of
the functional deficiency of Peyer's patches is Crohn's
disease, an inflammatory bowel disease characterized
by chronic or relapsing inflammation.
Polymeric IgA
Plasma cells secrete polymeric IgA into the intestinal lumen, the respiratory epithelium, the lactating mammary gland, and salivary glands. Most plasma cells are
present in the lamina propria of the intestinal villi,
together with lymphocytes, eosinophils, mast cells,
and macrophages.
Polymeric IgA molecules secreted by plasma cells
are transported from the lamina propria to the intestinal lumen by a transcytosis mechanism consisting
of the following steps:
1. Polymeric IgA is secreted as a dimeric molecule
joined by a peptide called the J chain.
2. Polymeric IgA binds to a specific receptor, called
the polymeric immunoglobulin receptor (pIgR),
available on the basal surfaces of the enterocytes. The
pIgR has an attached secretory component.
3. The polymeric IgA-pIgR-secretory component
complex is internalized and transported across the
cell to the apical surface of the epithelial cell.
4. At the apical surface, the complex is cleaved
enzymatically and the polymeric IgA-secretory component complex is released into the intestinal lumen as secreted IgA (SIgA). The secretory component protects the dimeric IgA from proteolytic degradation.
5. IgA attaches to bacteria and soluble antigens,
preventing a direct damaging effect to intestinal cells
and penetration into the lamina propria.
How are plasma cells induced to produce polymeric IgA?
When TLR on enterocytes is activated by microbiota, they secrete B cell-activating factor (BAF) and
a proliferation-inducing ligand (APRIL).
In the lamina propria, BAF and APRIL induce the
differentiation of B cells into IgA-producing plasma
cells.
In addition, the microbiota instructs enterocytes
through thymic stromal lymphoprotein (TSLP) to
engage dendritic cells in the lamina propria to secrete
BAF and APRIL and induce the differentiation of B
cells into plasma cells.
One last point: IgA regulates the composition and
the function of the intestinal microbiota by affecting
bacterial gene expression. By this mechanism, IgA keeps a congenial relationship between the host and
the microbiota.
In the discussion of Peyer's patches, it is indicated that M cells express IgA receptors allowing the uptake
of IgA-bound bacteria. It is realized that luminal SIgA
not only immobilize bacteria but also redirects them
to the M cells for internalization and disposal.
Paneth cells
Enterocytes and Paneth cells in particular secrete
proteins to limit bacteria pathogenic challenges. We
discuss in Chapter 11. Integumentary System, how
epithelial antimicrobial proteins (AMPs) protect skin
surfaces against microorganisms. We continue the
discussion within the context of the antimicrobial
defense of the intestinal mucosa involving Paneth
cells and enterocytes.
Most AMPs inactivate or kill bacteria directly by
enzymatic degradation of the bacterial wall or by
disrupting the bacterial inner membrane. A group
of AMPs deprive bacteria of essential heavy metal
such as iron.
AMPs produced by Paneth cells and enterocytes are
retained in the intestinal mucus blanket produced
by goblet cells. Therefore, the mucus layer protects
the intestinal mucosa by two mechanisms:
1. By creating a barrier that limits direct access of
luminal bacteria to the epithelium.
2. By concentrating AMPs near the enterocyte
surface. AMPs are virtually absent from the luminal
content.
Paneth cells are present at the base of the crypts
of Lieberkühn and have a lifetime of about 20 days.
The pyramid-shaped Paneth cells have a basal domain containing the rough endoplasmic reticulum.
The apical region shows numerous protein granules
representing a diverse array of AMPs, an indication of
the microbial diversity and impending threats (Figures
16-16 and 16-17).
Paneth cells produce several AMPs:
1. Defensins (_-defensin 5 [DEFA5] and _-
defensin 6 [DEFA6] in humans)
2. C-type lectins, including regenerating isletderived protein 3a (REG3a), also known as hepatointestinal protein/pancreatitis-associated protein
(HIP/PAP).
3. Lysozyme and phospholipase A2 (PLA2).
4. Angiogenin 4 (ANG4).
_-Defensins (2–3 kd) target Gram-positive and
Gram-negative bacteria, fungi, viruses, and protozoa
to produce membrane disruption by the formation of
defensin pores. Pores cause swelling and membrane
rupture enabling the entrance of water into the pathogen. Defensins can also be chemotactic to CD4+ T
cells, CD8+ T cells, monocytes, and macrophages
and modulate an inflammatory response. Defensins enhance the recruitment of dendritic cells to the site
of infection and facilitate the uptake of antigens by
forming defensin-antigen complexes.
Like all C-type lectins, the carbohydrate-recognition domain of REG3a
HIP/PAP (15 kd) binds
to the glycan chain of peptidoglycan present in the
bacterial cell wall of Gram-positive bacteria and
causes wall disruption. Peptidoglycan is present in
bacteria but not in human cells.
Recall that selectins, a member of the group of
Ca2+-dependent cell adhesion molecules, belong
to the C-type lectin family that have carbohydrate recognition domains.
Lysozyme is a proteolytic enzyme that cleaves
glycosidic linkages that maintain the integrity of cell
wall peptidoglycan. PLA2 kills bacteria by hydrolysis
of phospholipids in the bacterial membrane.
Paneth cells secrete ANG4, an RNAse with bactericidal properties.
It is important to emphasize that the expression and
function of AMPs are highly regulated by the presence or absence of the microbiota (see Figure 16-16).
In the presence of microorganisms:
1. TLR in enterocytes controls the expression of
REG3a/HIP/PAP through the TLR-signaling adaptor myeloid-differentiation primary response protein
88 (MYD88).
2. Cytoplasmic NOD2, expressed by Paneth cells,
controls the expression of _-defensins when it binds
to an internalized peptidoglycan peptide fragment
(muramyl dipeptide, MDP) and activates the transcription factor NF-gB.
Note that NOD2 is in a strategic position to
contribute to immunogenic tolerance toward the
microbiota when confronting MDP: NOD2 can
also limit the development of a CD4+ Tcell-initiated
immune response. However, _-defensins can be expressed independently of the microbiota by activation
of the transcription factor TCF4.
Defensins are produced continuously or in response to microbial products or proinflammatory
cytokines (for example, TNF ligand). As mentioned
in our discussion on the intestinal tight junction
barrier, TNF ligand is a proinflammatory cytokine
produced in response to diverse infectious agents
and tissue injury.
In summary, enterocytes and Paneth cells produce
a diverse group of AMPs that directly kill or inhibit
the growth of pathogenic microorganisms that can
contribute to inflammatory bowel diseases.
Pathology: Inflammatory bowel diseases
Inflammatory bowel disease includes ulcerative colitis and Crohn’s disease. Both are clinically characterized by diarrhea, pain, and periodic relapses.
Ulcerative colitis affects the mucosa of the large intestine. Crohn’s disease affects any segment of the
intestinal tract.
Crohn’s disease is a chronic inflammatory process
involving the terminal ileum but is also observed in
the large intestine. Inflammatory cells (neutrophils,
lymphocytes, and macrophages) produce cytokines
that cause damage to the intestinal mucosa (Figure
16-18).
The initial alteration of the intestinal mucosa
consists in the infiltration of neutrophils into the
crypts of Lieberkühn. This process results in the
destruction of the intestinal glands by the formation
of crypt abscesses and the progressive atrophy and
ulceration of the mucosa.
The chronic inflammatory process infiltrates the
submucosa and muscularis. Abundant accumulation
of lymphocytes forms aggregates of cells, or granulomas, a typical feature of Crohn’s disease.
Major complications of the disease are occlusion of
the intestinal lumen by fibrosis and the formation
of fistulas in other segments of the small intestine,
and intestinal perforation. Segments affected by
Crohn’s disease are separated by normal stretches of
intestinal segments.
The cause of Crohn’s disease is unknown. There is
increasing evidence suggesting that the disease arises
from dysregulated interactions between microorganisms and the intestinal epithelium involving NOD2.
Patients with intestinal bowel disease have an
increased number of bacteria associated with the epithelial cell surface, suggesting a failure of mechanisms
limiting direct contact between microorganisms and
the epithelium.
A contributing factor is the reactive immune response of the intestinal mucosa determined by an abnormal signaling exchange with the resident bacteria
(microbiota). In genetically susceptible individuals,
inflammatory bowel disease occurs when the mucosal
immune machinery regards the microbiota present
in normal and healthy individuals as pathogenic and
triggers an immune response.
As discussed (see Figure 16-12), cytokines produced by helper T cells within the intestinal mucosa
cause a proinflammatory response that characterizes
inflammatory bowel disease. In Crohn’s disease, type
1 helper cells (TH1 cells) produce TNF ligand and
interferon-a. Because TNF ligand is a proinflammatory cytokine, antibodies to this cytokine are being
administered to patients with Crohn’s disease to attenuate proinflammatory activity.
Clinical significance: Malabsorption syndromes
Malabsorption syndromes are characterized by a deficit in the absorption of fats, proteins, carbohydrates,
salts, and water by the mucosa of the small intestine.
Malabsorption syndromes can be caused by:
1. Abnormal digestion of fats and proteins by
pancreatic diseases (pancreatitis or cystic fibrosis) or
lack of solubilization of fats by defective bile secretion (hepatic disease or obstruction of the flow of bile
into the duodenum).
2. Enzymatic abnormalities at the brush border,
where disaccharidases and peptidases cannot hydrolyze carbohydrates (lactose intolerance) and proteins,
respectively.
3. A defect in the transepithelial transport by
enterocytes.
Malabsorption syndromes affect many organ systems. Anemia occurs when vitamin B12, iron, and
other cofactors cannot be absorbed. Disturbances of the musculoskeletal system are observed when proteins, calcium, and vitamin D fail to be absorbed. A
typical clinical feature of malabsorption syndromes
is diarrhea.