Main Model

Colon : Outer mucous tissue
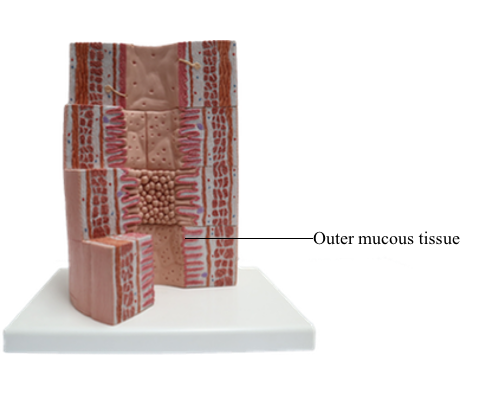
Large Intestine
The large intestine is formed by several successive
segments:
1. The cecum, projecting from which is the appendix.
2. The ascending, transverse, and descending
colon.
3. The sigmoid colon.
4. The rectum.
5. The anus.
Plicae circulares and intestinal villi are not found
beyond the ileocecal valve. Numerous openings of
the straight tubular glands or crypts of Lieberkühn
are characteristic of the mucosa of the colon.
The lining of the tubular glands of the colon
consists of the following:
1. A surface simple columnar epithelium formed
by absorptive enterocytes and goblet cells. Enterocytes have short apical microvilli, and the cells participate in the transport of ions and water. All regions
of the colon absorb Na+ and Cl– ions facilitated by
plasma membrane channels that are regulated by
mineralocorticoids. Aldosterone increases the number of Na+ channels and increases the absorption of Na+. Na+ ions entering the absorptive enterocytes are extruded by an Na+ pump. Goblet cells secrete
mucus to lubricate the mucosal surface and serve as
a protective barrier.
2. A glandular epithelium, lining the glands or
crypts of Lierberkühn, consists of enterocytes and
predominant goblet cells, stem cells, and dispersed
enteroendocrine cells. Paneth cells may be present
in the cecum.
A lamina propria and a muscularis mucosae are
present, as are isolated lymphoid follicles (ILFs)
penetrating the submucosa. Glands are not present
in the submucosa. Unlike Peyer's patches, ILFs are
not associated with M cells.
The muscularis has a particular feature: The
bundles of its outer longitudinal layer fuse to form the taeniae coli. The taeniae coli consist of three
longitudinally oriented ribbon-like bands, each 1
cm wide. The contraction of the taeniae coli and
circular muscle layer draws the colon into sacculations called haustra.
The serosa has scattered sacs of adipose tissue, the
appendices epiploicae, which is a unique feature,
together with the haustra, of the colon.
The Appendix
The appendix is a diverticulum of
the cecum and has layers similar to those of the large intestine. The characteristic features of the appendix
are the lymphoid tissue, represented by multiple lymphatic follicles, and lymphocytes infiltrating the
lamina propria. Lymphatic follicles extend into the
mucosa and submucosa and disrupt the continuity
of the muscularis mucosae. The submucosa contains
adipocytes and dense irregular connective tissue.
The inner circular layers of the muscularis is well
developed in contrast with the outer longitudinal
layer covered by the serosa.
The Rectum
The rectum, the terminal portion of the intestinal
tract, is a continuation of the sigmoid colon. The
rectum consists of two parts:
1. The upper part, or rectum proper.
2. The lower part, or anal canal.
The mucosa is thicker, with prominent veins, and
the crypts of Lieberkühn are longer (0.7 mm) than
in the small intestine and lined predominantly by
goblet cells. At the level of the anal canal, the crypts
gradually disappear and the serosa is replaced by an
adventitia.
A characteristic feature of the mucosa of the anal
canal are 8 to 10 longitudinal anal columns. The
base of the anal columns is the pectinate line. The
anal columns are connected at their base by valves,
corresponding to transverse folds of the mucosa. Small pockets, called anal sinuses, or crypts, are
found behind the valves. Anal mucous glands open
into each sinus.
The valves and sinuses prevent leakage from the
anus. When the canal is distended with feces, the
columns, sinuses, and valves flatten, and mucus is
discharged from the sinuses to lubricate the passage
of the feces.
Beyond the pectinate line, the simple columnar epithelium of the rectal mucosa is replaced by a stratified
squamous epithelium. This epithelial transformation
zone has clinical significance in pathology: colorectal
adenocarcinoma (gland-like) originates above the
transformation zone; epidermoid (epidermis-like)
carcinoma originates below the transformation zone
(anal canal).
At the level of the anus, the inner circular layer
of smooth muscle thickens to form the internal anal
sphincter. The longitudinal smooth muscle layer extends over the sphincter and attaches to the connective
tissue. Below this zone, the mucosa consists of stratified squamous epithelium with a few sebaceous and
sweat glands in the submucosa (circumanal glands
similar to the axillary sweat glands). The external anal
sphincter is formed by skeletal muscle and lies inside
the levator ani muscle, also with a sphincter function.
Pathology: Hirschsprung's Disease
During formation of the neural tube, neural crest
cells migrate from the neuroepithelium along defined
pathways to tissues, where they differentiate into
various cell types.
One destination of neural crest cells is the alimentary tube, where they develop the enteric nervous
system. The enteric nervous system partially controls
and coordinates the normal movements of the alimentary tube that facilitate digestion and transport
of bowel contents.
The large intestine, like the rest of the alimentary
tube, is innervated by the enteric nervous system
receiving impulses from extrinsic parasympathetic
and sympathetic nerves and from receptors within
the large intestine.
The transit of contents from the small intestine to
the large intestine is intermittent and regulated at the
ileocecal junction by a sphincter mechanism: When
the sphincter relaxes, ileal contractions propel the
contents into the large intestine.
Segmental contractions in an orad-to-aborad direction move the contents over short distances. The
material changes from a liquid to a semisolid state
when it reaches the descending and sigmoid colon.
The rectum is usually empty.
Contraction of the inner anal sphincter closes the
anal canal. Defecation occurs when the sphincter relaxes as part of the rectosphincteric reflex stimulated
by distention of the rectum.
Delayed transit through the colon leads to severe
constipation. An abnormal form of constipation is
seen in Hirschsprung's disease (congenital megacolon) caused by the absence of the enteric nervous system in a segment of the distal colon.
This condition, called aganglionosis, results from
an arrest in the migration of cells from the neural
crest, the precursors of the intramural ganglion cells
of the plexuses of Meissner and Auerbach. Aganglionosis is caused by mutations of the RET gene
encoding a receptor tyrosine kinase.
RET signaling is required for:
1. The formation of Peyer's patches.
2. The migration of neural crest cells into the distal
portions of the large intestine.
3. The differentiation of neural crest cells into
neurons of the enteric nervous system.
The permanently contracted aganglionic segment
does not allow the entry of the contents. An increase
in muscular tone in the orad segment results in its dilation, thus generating a megacolon or megarectum.
This condition is apparent shortly after birth when
the abdomen of the infant becomes distended and
little meconium is eliminated.
The diagnosis is confirmed by a biopsy of the
mucosa and submucosa of the rectum showing thick
and irregular nerve bundles, abundant acetylcholinesterase detected by immunohistochemistry and a
lack of ganglion cells.
Surgical removal of the affected colon segment is
the treatment of choice but intestinal dysfunction
may persist after surgery.
Pathology: Colorectal Tumorigenesis
Colorectal tumors develop from a polyp, a tumoral mass that protrudes into the lumen of the intestine.
Some polyps are non-neoplastic and are relatively
common in persons 60 years and older. Polyps can
be present in large number (100 or more) in familial
polyposis syndromes such as familial adenomatous
polyposis (FAP) and the Peutz-Jeghers syndrome.
FAP is determined by autosomal dominant mutations, in particular in the APC (adenomatous polyposis coli) gene. FAP patients develop multiple
polyps in the colon in their teenage years, increase in
number with age and later become cancerous.
Mutations in the APC gene have been detected in
85% of colon tumors, indicating that, as with the
retinoblastoma (Rb) gene, the inherited gene is also
important in the development of the sporadic form
of the cancer.
The APC gene encodes APC protein with binding affinity to beta-catenin, a molecule associated with
a catenin complex linked to E-cadherin and also a transcriptional
coactivator.
Mutations in the APC gene have also been found
in people with desmoid tumors, a benign tumor of
the connective tissue. Mutations in the APC gene
are also observed in Turcot syndrome, characterized
by an association of colorectal cancer with medulloblastoma, a brain tumor. The APC gene is located
on the long (q) arm of chromosome 5.
When beta-catenin is not part of the catenin complex:
1. Free cytoplasmic beta-catenin can be phosphorylated by glycogen synthase kinase 3beta (GSK3beta) (coassembled with proteins APC, axin and casein kinase
Ialpha, CKIalpha) and targeted for proteasomal degradation.
Phosphorylated beta-catenin is recognized by a ubiquitin ligase complex that catalyzes the attachment of
polyubiquitin chains to phosphorylated beta-catenin. Polyubiquitin conjugates of beta-catenin are rapidly
degraded by the 26S proteasome.
2. Alternatively, free cytoplasmic beta-catenin can
enter the nucleus and interact with the transcription factors TCF (T cell factor) and LEF (lymphoid
enhancer factor) to stimulates transcription of target
genes.
A mutation in the APC gene results in a truncated nonfunctional protein unable to interact with beta-catenin and initiate its disposal when is no longer
needed. Essentially, APC behaves as a tumor suppressor gene.
The APC gene is also a major regulator of the Wnt
pathway, a signaling system expressed during early
development and embryogenesis. Wnt proteins can inactivate GSK3beta, prevent the phosphorylation of beta-catenin, and abrogate
its destruction by the 26S proteasome. Consequently,
an excess of beta-catenin translocates to the cell nucleus
to affect gene transcription.
A defective beta-catenin pathway can overexpress
the microphthalmia-associated transcription factor
(MITF). The MITF is significant in the survival and
proliferation of melanoma cells.
Hereditary nonpolyposis colon cancer (HNPCC;
Lynch syndrome) is an inherited form of colorectal
cancer caused by mutations in DNA mismatch
repair, MMR, genes, involved in the repair of DNA
defects.
Mutation analysis of MMR genes (including
MLH1, MSH2, MSH6, PMS2, and EPCAM genes)
by microsatellite instability (MIS) screening testing
using colon tumor tissue removed by colonoscopy
or surgery, is carried out when there is evidence
of a DNA repair defect in a tumor. Note that not
all individuals who carry these mutations develop
cancerous tumors.
DNA repair defects increase the frequency of somatic mutations leading to malignant transformation.
HNPCC is an example of a cancer syndrome caused
by mutations in DNA repair proteins.
Patients with the HNPCC syndrome do not show
the very large number of colon polyps typical of the
familial polyposis syndrome, but a small number of
polyps occur frequently among gene carriers.