Main Model

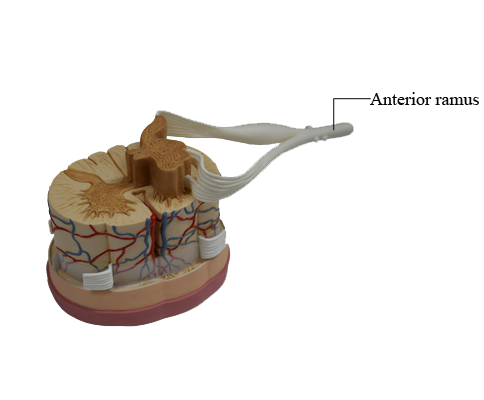
Anterior : Anterior ramus
Types of Nerves
The peripheral nervous system (PNS) is anatomically and operationally continuous with the central nervous system (CNS). Its afferent (sensory) fibers convey neural impulses to the CNS from the sense organs (e.g., the eyes) and from sensory receptors in various parts of the body (e.g., in the skin). Its efferent (motor) fibers convey neural impulses from the CNS to effector organs (muscles and glands).
Nerves are either cranial nerves or spinal nerves, or derivatives of them.
• Cranial nerves exit the cranial cavity through foramina (openings) in the cranium (Greek kranion, skull) and are identified by a descriptive name (e.g., “trochlear nerve”) or a Roman numeral (e.g., “CN IV”). Only 11 of the 12 pairs of cranial nerves arise from the brain; the other pair (CN XI) arises from the superior part of the spinal cord.
• Spinal (segmental) nerves exit the vertebral column (spine) through intervertebral foramina. Spinal nerves arise in bilateral pairs from a specific segment of the spinal cord. The 31 spinal cord segments and the 31 pairs of nerves arising from them are identified by a letter and number (e.g., “T4”) designating the region of the spinal cord and their superior-to-inferior order (C, cervical; T, thoracic; L, lumbar; S, sacral; Co, coccygeal).
Spinal Nerves
Spinal nerves initially arise from the spinal cord as rootlets (a detail commonly omitted from diagrams for the sake of simplicity); the rootlets converge to form two nerve roots:
1. An anterior (ventral) nerve root, consisting of motor (efferent) fibers passing from nerve cell bodies in the anterior horn of spinal cord gray matter to effector organs located peripherally.
2. A posterior (dorsal) nerve root, consisting of sensory (afferent) fibers from cell bodies in the spinal (sensory) or posterior (dorsal) root ganglion (commonly abbreviated in clinical use as “DRG”) that extend peripherally to sensory endings and centrally to the posterior horn of spinal cord gray matter.
The posterior and anterior nerve roots unite, within or just proximal to the intervertebral foramen, to form a mixed (both motor and sensory) spinal nerve, which immediately divides into two rami (Latin, branches): a posterior (dorsal) ramus and an anterior (ventral) ramus. As branches of the mixed spinal nerve, the posterior and anterior rami carry both motor and sensory fibers, as do all their subsequent branches. The terms motor nerve and sensory nerve are almost always relative terms, referring to the majority of fiber types conveyed by that nerve. Nerves supplying muscles of the trunk or limbs (motor nerves) also contain about 40% sensory fibers, which convey pain and proprioceptive information. Conversely, cutaneous (sensory) nerves contain motor fibers, which serve sweat glands and the smooth muscle of blood vessels and hair follicles.
The unilateral area of skin innervated by the sensory fibers of a single spinal nerve is called a dermatome; the unilateral muscle mass receiving innervation from the fibers conveyed by a single spinal nerve is a myotome. From clinical studies of lesions of the posterior roots or spinal nerves, dermatome maps have been devised to indicate the typical pattern of innervation of the skin by specific spinal nerves. However, a lesion of a single posterior root or spinal nerve would rarely result in numbness over the area demarcated for that nerve in these maps because the fibers conveyed by adjacent spinal nerves overlap almost completely as they are distributed to the skin, providing a type of double coverage. The lines indicating dermatomes on dermatome maps would thus be better represented by smudges or gradations of color. Generally, at least two adjacent spinal nerves (or posterior roots) must be interrupted to produce a discernible area of numbness.
As they emerge from the intervertebral foramina, spinal nerves are divided into two rami:
1. Posterior (primary) rami of spinal nerves supply nerve fibers to the synovial joints of the vertebral column, deep muscles of the back, and the overlying skin in a segmental pattern. As a general rule, the posterior rami remain separate from each other (do not merge to form major somatic nerve plexuses).
2. Anterior (primary) rami of spinal nerves supply nerve fibers to the much larger remaining area, consisting of the anterior and lateral regions of the trunk and the upper and lower limbs. The anterior rami that are distributed exclusively to the trunk generally remain separate from each other, also innervating muscles and skin in a segmental pattern. However, primarily in relationship to the innervation of the limbs, the majority of anterior rami merge with one or more adjacent anterior rami, forming the major somatic nerve plexuses (networks) in which their fibers intermingle and from which a new set of multisegmental peripheral nerves emerges. The anterior rami of spinal nerves participating in plexus formation contribute fibers to multiple peripheral nerves arising from the plexus; conversely, most peripheral nerves arising from the plexus contain fibers from multiple spinal nerves.
Although the spinal nerves lose their identity as they split and merge in the plexus, the fibers arising from a specific spinal cord segment and conveyed from it by a single spinal nerve are ultimately distributed to one segmental dermatome, although they may reach it by means of a multisegmental peripheral nerve arising from the plexus that also conveys fibers to all or parts of other adjacent dermatomes.
It is therefore important to distinguish between the distribution of the fibers carried by spinal nerves (segmental innervation or distribution - i.e., dermatomes and myotomes labeled with a letter and a number, such as “T4”) and of the fibers carried by branches of a plexus (peripheral nerve innervation or distribution, labeled with the names of peripheral nerves, such as “the median nerve”). Mapping segmental innervation (dermatomes determined by clinical experience) and mapping the distribution of peripheral nerves (determined by dissecting the branches of a named nerve distally) produce entirely different maps, except for most of the trunk where, in the absence of plexus formation, segmental and peripheral distributions are the same. The overlapping in the cutaneous distribution of nerve fibers conveyed by adjacent spinal nerves also occurs in the cutaneous distribution of nerve fibers conveyed by adjacent peripheral nerves.
Cranial Nerves
As they arise from the CNS, some cranial nerves convey only sensory fibers, some only motor fibers, and some carry a mixture of both types of fibers. Communication occurs between cranial nerves, and between cranial nerves and upper cervical (spinal) nerves; thus a nerve that initially conveys only motor fibers may receive sensory fibers distally in its course, and vice versa. Except for the first two (those involved in the senses of smell and sight), cranial nerves that convey sensory fibers into the brain bear sensory ganglia (similar to spinal or posterior root ganglia), where the cell bodies of the pseudounipolar fibers are located. Although, by definition, the term dermatome applies only to spinal nerves, similar areas of skin supplied by single cranial nerves can be identified and mapped. Unlike dermatomes, however, there is little overlap in the innervation of zones of skin supplied by cranial nerves.
Somatic and Visceral Fibers
The types of fibers conveyed by cranial or spinal nerves are as follows:
• Somatic fibers
• General sensory fibers (general somatic afferent [GSA] fibers) transmit sensations from the body to the CNS; they may be exteroceptive sensations from the skin (pain, temperature, touch, and pressure) or pain and proprioceptive sensations from muscles, tendons, and joints. Proprioceptive sensations are usually subconscious, providing information regarding joint position and the tension of tendons and muscles. This information is combined with input from the vestibular apparatus of the internal ear, resulting in awareness of the orientation of the body and limbs in space, independent of visual input.
• Somatic motor fibers (general somatic efferent [GSE] fibers) transmit impulses to skeletal (voluntary) muscles.
• Visceral fibers
• Visceral sensory fibers (general visceral afferent [GVA] fibers) transmit pain or subconscious visceral reflex sensations (information concerning distension, blood gas, and blood pressure levels, for example) from hollow organs and blood vessels to the CNS.
• Visceral motor fibers (general visceral efferent [GVE] fibers) transmit impulses to smooth (involuntary) muscle and glandular tissues. Two varieties of fibers, presynaptic and postsynaptic, work together to conduct impulses from the CNS to smooth muscle or glands.
Both types of sensory fibers - visceral sensory and general sensory - are processes of pseudounipolar neurons with cell bodies located outside of the CNS in spinal or cranial sensory ganglia. The motor fibers of nerves are axons of multipolar neurons. The cell bodies of somatic motor and presynaptic visceral motor neurons are located in the gray matter of the spinal cord. Cell bodies of postsynaptic motor neurons are located outside the CNS in autonomic ganglia.
In addition to the fiber types listed above, some cranial nerves also convey special sensory fibers for the special senses (smell, sight, hearing, balance, and taste). On the basis of the embryologic/phylogenetic derivation of certain muscles of the head and neck, some motor fibers conveyed by cranial nerves to striated muscle have traditionally been classified as “special visceral”; however, since the designation is confusing and not applied clinically, that term will not be used here. These fibers are occasionally designated as branchial motor, referring to muscle tissue derived from the pharyngeal arches in the embryo.