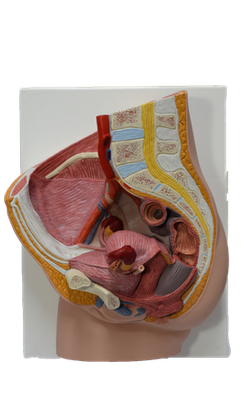
Main Model
16 Vagina

The female internal genital organs include the ovaries, uterine tubes, uterus, and vagina.
The vagina, a distensible musculomembranous tube (7-9 cm long), extends from the middle cervix of the uterus to the vaginal orifice, the opening at the inferior end of the vagina. The vaginal orifice, external urethral orifice, and ducts of the greater and lesser vestibular glands open into the vestibule of the vagina, the cleft between the labia minora. The vaginal part of the cervix lies anteriorly in the superior vagina.
The vagina:
• serves as a canal for menstrual fluid.
• forms the inferior part of the birth canal.
• receives the penis and ejaculate during sexual intercourse.
• communicates superiorly with the cervical canal and inferiorly with the vestibule of the vagina.
The vagina is usually collapsed. The orifice is usually collapsed toward the midline so that its lateral walls are in contact on each side of an anteroposterior slit. Superior to the orifice, however, the anterior and posterior walls are in contact on each side of a transverse potential cavity, H-shaped in cross section, except at its superior end where the cervix holds them apart. The vagina lies posterior to the urinary bladder and urethra, the latter projecting along the midline of its inferior anterior wall. The vagina lies anterior to the rectum, passing between the medial margins of the levator ani (puborectalis) muscles. The vaginal fornix, the recess around the cervix, has anterior, posterior, and lateral parts. The posterior vaginal fornix is the deepest part and is closely related to the recto-uterine pouch. Four muscles compress the vagina and act as sphincters: pubovaginalis, external urethral sphincter, urethrovaginal sphincter, and bulbospongiosus.
The vagina is related:
• anteriorly to the fundus of the urinary bladder and urethra.
• laterally to the levator ani, visceral pelvic fascia, and ureters.
• posteriorly (from inferior to superior) to the anal canal, rectum, and recto-uterine pouch.
The arteries supplying the superior part of the vagina derive from the uterine arteries. The arteries supplying the middle and inferior parts of the vagina derive from the vaginal and internal pudendal arteries.
The vaginal veins form vaginal venous plexuses along the sides of the vagina and within the vaginal mucosa. These veins are continuous with the uterine venous plexus as the uterovaginal venous plexus, and drain into the internal iliac veins through the uterine vein. This plexus also communicates with the vesical and rectal venous plexuses.
Only the inferior one fifth to one quarter of the vagina is somatic in terms of innervation. Innervation of this part of the vagina is from the deep perineal nerve, a branch of the pudendal nerve, which conveys sympathetic and visceral afferent fibers but no parasympathetic fibers. Only this somatically innervated part is sensitive to touch and temperature, even though the somatic and visceral afferent fibers have their cell bodies in the same (S2-S4) spinal ganglia.
Most of the vagina (superior three quarters to four fifths) is visceral in terms of its innervation. Nerves to this part of the vagina and to the uterus are derived from the uterovaginal nerve plexus, which travels with the uterine artery at the junction of the base of the (peritoneal) broad ligament and the superior part of the (fascial) transverse cervical ligament. The uterovaginal nerve plexus is one of the pelvic plexuses that extends to the pelvic viscera from the inferior hypogastric plexus. Sympathetic, parasympathetic, and visceral afferent fibers pass through this plexus.
Sympathetic innervation originates in the inferior thoracic spinal cord segments and passes through lumbar splanchnic nerves and the intermesenteric-hypogastric-pelvic series of plexuses. Parasympathetic innervation originates in the S2-S4 spinal cord segments and passes through the pelvic splanchnic nerves to the inferior hypogastric-uterovaginal plexus. The visceral afferent innervation of the superior (intraperitoneal; fundus and body) and inferior (subperitoneal; cervical) parts of the uterus and vagina differ in terms of course and destination. Visceral afferent fibers conducting pain impulses from the intraperitoneal uterine fundus and body (superior to the pelvic pain line) follow the sympathetic innervation retrograde to reach cell bodies in the inferior thoracic-superior lumbar spinal ganglia. Afferent fibers conducting pain impulses from the subperitoneal uterine cervix and vagina (inferior to the pelvic pain line) follow the parasympathetic fibers retrograde through the uterovaginal and inferior hypogastric plexuses and pelvic splanchnic nerves to reach cell bodies in the spinal sensory ganglia of S2-S4. The two different routes followed by visceral pain fibers is clinically significant in that it offers mothers a variety of types of anesthesia for childbirth. All visceral afferent fibers from the uterus and vagina not concerned with pain (those conveying unconscious sensations) also follow the latter route.