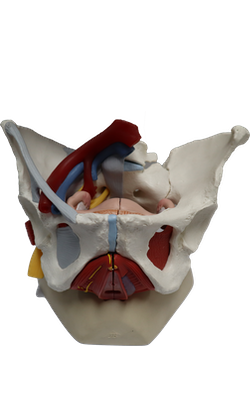
Main Model
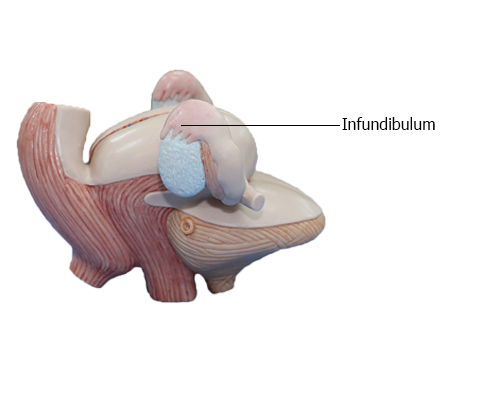
FEMALE INTERNAL GENITAL ORGANS : Infundibulum
Uterine Tubes
The uterine tubes (formerly called oviducts or fallopian tubes) conduct the oocyte, discharged monthly from an ovary during child-bearing years, from the peri-ovarian peritoneal cavity to the uterine cavity. They also provide the usual site of fertilization. The tubes extend laterally from the uterine horns and open into the peritoneal cavity near the ovaries.
The uterine tubes (approximately 10 cm long) lie in a narrow mesentery, the mesosalpinx, forming the free anterosuperior edges of the broad ligaments. In the "ideal" disposition, as typically illustrated, the tubes extend symmetrically posterolaterally to the lateral pelvic walls, where they arch anterior and superior to the ovaries in the horizontally disposed broad ligament. In reality, as seen in an ultrasound examination, the tubes are commonly asymmetrically arranged with one or the other often lying superior and even posterior to the uterus.
The uterine tubes are divisible into four parts, from lateral to medial:
(1) Infundibulum: the funnel-shaped distal end of the tube that opens into the peritoneal cavity through the abdominal ostium. The finger-like processes of the fimbriated end of the infundibulum (fimbriae) spread over the medial surface of the ovary; one large ovarian fimbria is attached to the superior pole of the ovary.
(2) Ampulla: the widest and longest part of the tube, which begins at the medial end of the infundibulum; fertilization of the oocyte usually occurs in the ampulla.
(3) Isthmus: the thick-walled part of the tube, which enters the uterine horn.
(4) Uterine part: the short intramural segment of the tube that passes through the wall of the uterus and opens via the uterine ostium into the uterine cavity at the uterine horn.
Arterial Supply and Venous Drainage of Ovaries and Uterine Tubes
The ovarian arteries arise from the abdominal aorta and descend along the posterior abdominal wall. At the pelvic brim, they cross over the external iliac vessels and enter the suspensory ligaments, approaching the lateral aspects of the ovaries and uterine tubes. The ascending branches of the uterine arteries (branches of the internal iliac arteries) course along the lateral aspects of the uterus to approach the medial aspects of the ovaries and tubes. Both the ovarian and ascending uterine arteries terminate by bifurcating into ovarian and tubal branches, which supply the ovaries and tubes from opposite ends and anastomose with each other, providing a collateral circulation from abdominal and pelvic sources to both structures.
Veins draining the ovary form a vine-like pampiniform plexus of veins in the broad ligament near the ovary and uterine tube. The veins of the plexus usually merge to form a singular ovarian vein, which leaves the lesser pelvis with the ovarian artery. The right ovarian vein ascends to enter the inferior vena cava; the left ovarian vein drains into the left renal vein. The tubal veins drain into the ovarian veins and uterine (uterovaginal) venous plexus.
Innervation of Ovaries and Uterine Tubes
The nerve supply derives partly from the ovarian plexus, descending with the ovarian vessels, and partly from the uterine (pelvic) plexus. The ovaries and uterine tubes are intraperitoneal and, therefore, are superior to the pelvic pain line. Thus, visceral afferent pain fibers ascend retrogradely with the descending sympathetic fibers of the ovarian plexus and lumbar splanchnic nerves to cell bodies in the T11-L1 spinal sensory ganglia. Visceral afferent reflex fibers follow parasympathetic fibers retrogradely through the uterine (pelvic) and inferior hypogastric plexuses and the pelvic splanchnic nerves to cell bodies in the S2-S4 spinal sensory ganglia.