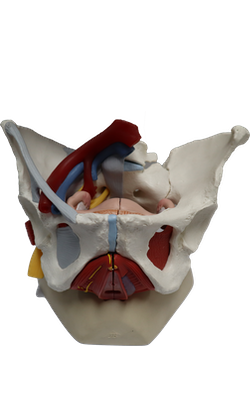
Main Model
FEMALE INTERNAL GENITAL ORGANS : Ovary
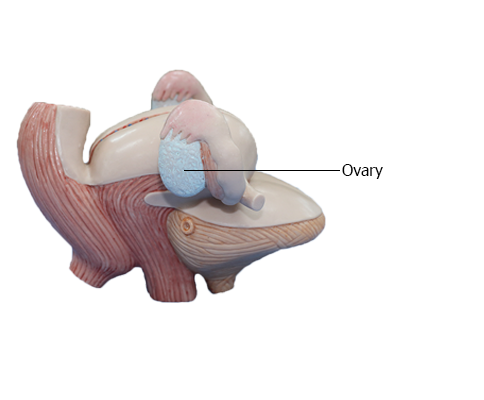
Ovaries
The ovaries are almond-shaped and -sized female gonads in
which the oocytes (female gametes or germ cells) develop. They
are also endocrine glands that produce reproductive hormones.
Each ovary is suspended by a short peritoneal fold or mesentery,
the mesovarium. The mesovarium is a subdivision
of a larger mesentery of the uterus, the broad ligament.
In prepubertal females, the connective tissue capsule (tunica
albuginea of the ovary) comprising the surface of the ovary is
covered by a smooth layer of ovarian mesothelium or surface
(germinal) epithelium, a single layer of cuboidal cells that gives
the surface a dull, grayish appearance, contrasting with the shiny
surface of the adjacent peritoneal mesovarium with which it is
continuous. After puberty, the ovarian surface epithelium becomes progressively scarred and distorted because of
the repeated rupture of ovarian follicles and discharge of oocytes
during ovulation. The scarring is less in women who have been
taking oral contraceptives that inhibit ovulation.
The ovarian vessels, lymphatics, and nerves cross the pelvic
brim, passing to and from the superolateral aspect of the ovary
within a peritoneal fold, the suspensory ligament of the
ovary, which becomes continuous with the mesovarium of the
broad ligament. Medially within the mesovarium, a short ligament of ovary tethers the ovary to the uterus. Consequently
the ovaries are typically found laterally between the uterus
and the lateral pelvic wall during a manual or ultrasonic pelvic
examination. The ligament of ovary is a remnant
of the superior part of the ovarian gubernaculum of the fetus. The ligament of the ovary connects the proximal (uterine) end of the ovary to the lateral angle of
the uterus, just inferior to the entrance of the uterine tube. Because the ovary is suspended in the peritoneal cavity and its surface is not covered by peritoneum, the
oocyte expelled at ovulation passes into the peritoneal cavity. However, its intraperitoneal life is short because it is normally
trapped by the fimbriae of the infundibulum of the uterine
tube and carried into the ampulla, where it may be fertilized.
Arterial Supply and Venous Drainage of Ovaries
and Uterine Tubes
The ovarian arteries arise from the
abdominal aorta and descend
along the posterior abdominal wall. At the pelvic brim, they
cross over the external iliac vessels and enter the suspensory ligaments, approaching the lateral aspects
of the ovaries and uterine tubes. The ascending branches of
the uterine arteries (branches of the internal iliac arteries)
course along the lateral aspects of the uterus to approach
the medial aspects of the ovaries and tubes. Both the ovarian and ascending uterine arteries terminate by bifurcating into ovarian and tubal branches, which supply the ovaries and tubes from opposite ends and anastomose with each other, providing a collateral circulation from
abdominal and pelvic sources to both structures.
Veins draining the ovary form a vine-like pampiniform plexus of veins in the broad ligament near the ovary
and uterine tube. The veins of the plexus usually merge to form a singular ovarian vein, which leaves
the lesser pelvis with the ovarian artery. The right ovarian
vein ascends to enter the inferior vena cava; the left ovarian vein drains into the left renal vein. The tubal
veins drain into the ovarian veins and uterine (uterovaginal)
venous plexus.
Innervation of Ovaries and Uterine Tubes
The
nerve supply derives partly from the ovarian plexus, descending with the ovarian vessels, and partly from the uterine
(pelvic) plexus. The ovaries and uterine tubes
are intraperitoneal and, therefore, are superior to the pelvic
pain line. Thus, visceral afferent pain fibers
ascend retrogradely with the descending sympathetic fibers
of the ovarian plexus and lumbar splanchnic nerves to cell
bodies in the T11-L1 spinal sensory ganglia. Visceral afferent reflex fibers follow parasympathetic fibers retrogradely
through the uterine (pelvic) and inferior hypogastric plexuses
and the pelvic splanchnic nerves to cell bodies in the S2-S4 spinal sensory ganglia.