Main Model
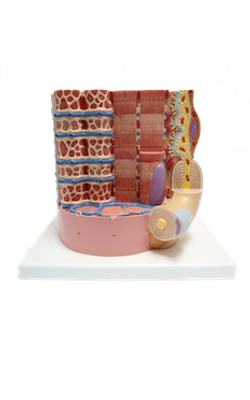
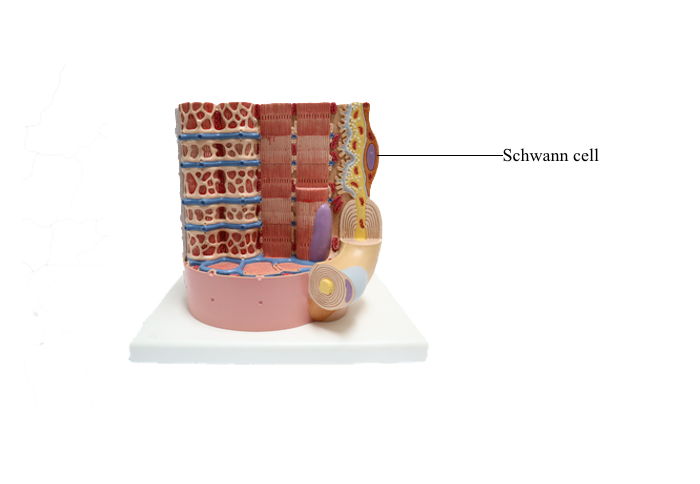
Anterior : Schwann cell
Peripheral Nervous System
The PNS includes all neuronal elements outside the
brain and spinal cord. The peripheral nerves are the
cranial and spinal nerves.
The PNS contains two supporting cell types:
1. Schwann cells, analogous to the oligodendrocytes of the CNS.
2. Satellite cells, Schwann cell - like surrounding
the cell bodies of neurons in sensory and autonomic
ganglia.
Individual nerve fibers of the PNS are ensheathed
by Schwann cells. In myelinated fibers, individual Schwann cells wrap around the axon,
forming a myelin sheath analogous to that of the
oligodendrocytes of the CNS. In
unmyelinated fibers, a single Schwann cell envelops several axons.
There are two important differences between
Schwann cells and oligodendrocytes:
1. A single Schwann cell forms only one internodal
segment of myelin, whereas a single oligodendrocyte
may form 40 or 50 internodes.
2. Unmyelinated fibers in the PNS are embedded
in Schwann cells, whereas those in the CNS are not
ensheathed by oligodendrocytes but may have an
investment of astrocytes.
Structure of a Peripheral Nerve
Connective tissue coverings divide the peripheral
nerve into three segments, each with unique structural characteristics:
1. The epineurium.
2. The perineurium.
3. The endoneurium.
The epineurium is formed by type I collagen and
fibroblasts and covers the entire nerve. It contains
arteries, veins and lymphatic vessels.
Within the nerve, the perineurium segregates axons into fascicles. The perineurium consists of several
concentric layers of neuroepithelial perineurial cells
with two distinct characteristics:
1. A basal lamina, consisting of type IV collagen
and laminin, surrounds the layers of perineurial cells.
2. Perineurial cells are joined to each other by tight
junctions to form a protective diffusion barrier: the
blood-nerve barrier, responsible for maintaining the physiologic microenvironment of the endoneurium.
The endoneurium surrounds individual axons and
their associated Schwann cells and myelin sheaths. It
consists of type III collagen fibrils, a few fibroblasts,
macrophages, mast cells and endoneurial capillaries
between individual the axons lor nerve fibers.
Multiple unmyelinated axons are individually
encased within recesses of the cytoplasm of Schwann
cells. Unmyelinated axons do not
undergo the spiral concentric lamination and myelin formation. For future reference in neuropathology,
keep in mind the Luxol fast blue staining method
widely used for myelin staining.
Additional components of the blood-nerve barrier
are the endothelial cells of the endoneurial capillaries. Endoneurial capillaries derive from the vasa
nervorum and are lined by continuous endothelial
cells joined by tight junctions.
Pathology: Schwannomas
Schwannomas are benign encapsulated tumors
consisting of Schwann cells. Keep in mind that Schwann cells are present in all peripheral nerves.
Therefore, schwannomas can be found in many sites
(intracranial, intraspinal and extraspinal locations).
Schwannomas can develop at the surface or inside
of a nerve fascicle and display spindle cells (called
Antoni A pattern) or multipolar cells (called Antoni
B pattern), the latter representing the result of a degenerative process. All schwannomas are immunoreactive for S-100 protein (a calmodulin-like cytosolic
protein present in cells derived from the neural crest),
type IV collagen and laminin. Schwannomas need
to be distinguished from neurofibromas, that may contain Schwann cells.
Pathology: Segmental Demyelination and Axonal Degeneration
Diseases affecting Schwann cells lead to a loss of
myelin, or segmental demyelination. Damage to
the neuron and its axon leads to axonal degeneration (wallerian degeneration, first described by the
English physiologist Augustus Volney Waller, 1816-1870).
Axonal degeneration may be followed by axonal regeneration. The motor
unit is the functional unit of the neuromuscular
system. Therefore, segmental demyelination and
axonal degeneration affect the motor unit and cause
muscle paralysis and atrophy. Physiotherapy for the paralyzed muscles is necessary to prevent muscle
degeneration before regenerating motor axons can
reach the motor unit.
Neurotrophins play a significant role in the survival of neurons uncoupled from a peripheral target.
Segmental demyelination occurs when the function of the Schwann cell is abnormal or there is damage to the myelin sheath, for example, a traumatic
nerve injury. If the nerve fiber is completely severed,
the chances of recovery decrease unless a nerve segment is grafted.
The presence of the endoneurium is essential for
the proliferation of Schwann cells. Schwann cells
guide an axonal sprout, derived from the proximal
axonal stump, to reach the end organ (for example,
a muscle).
Several sprouts can grow into the connective tissue
and, together with proliferative Schwann cells, form a
mass called an traumatic neuroma.
Traumatic neuromas prevent regrowth of the axon
after trauma and must be surgically removed to allow
reinnervation of the peripheral end organ.
Axonal regeneration is a very slow process. It starts
2 weeks after injury and is completed, if successful,
after several months. Schwann cells remyelinate the
denuded portion of the axon, but the length of internodal myelin is shorter.
Axonal degeneration results from the primary destruction of the axon by metabolic or toxic damage
and is followed by demyelination and degeneration
of the neuronal cell body. This process is known as a "dying back" neuropathy.
Regeneration of nerve fibers in the CNS is not
possible at present because of the following factors:
1. An endoneurium is not present.
2. Oligodendrocytes do not proliferate in contrast
to Schwann cells, and a single oligodendrocyte serves
a large number of axons.
3. Astrocytes deposit scar tissue (the astrocytic
plaque).
Sensory (Spinal) Ganglia
A cluster of neurons forms a ganglion (plural ganglia).
A ganglion can be sensory (dorsal root ganglia and
trigeminal ganglion) or motor (visceromotor or autonomic ganglia). Axons derived from a ganglion are
organized as nerves, rami (singular ramus), or roots.
Sensory ganglia of the posterior spinal nerve
roots and the trunks of the trigeminal, facial, glossopharyngeal, and vagal cranial nerves have a similar
organization.
A connective tissue capsule, representing the
continuation of the epineurium and perineurium, surrounds each ganglion.
Neurons are pseudounipolar, with a single stem
myelinated process leaving each cell body. The short
process bifurcates into a peripheral centrifugal branch
into one ramus of the spinal nerve and a centripetal
branch into the spinal cord.
The neuronal cell body is surrounded by a layer of
flattened satellite cells, similar to Schwann cells and
continuous with them as they enclose the peripheral and central process of each neuron.
Following stimulation of the peripheral sensory
receptor, nerve impulse reach the T-bifurcation junction bypassing the neuronal cell body, traveling from
the peripheral axon to the centripetal axon.