Main Model

Ileum
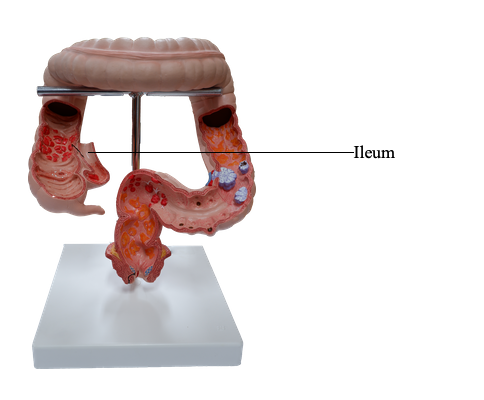
Jejunum and Ileum
The second part of the small intestine, the jejunum, begins
at the duodenojejunal flexure where the gastrointestinal
tract resumes an intraperitoneal course. The third part
of the small intestine, the ileum, ends at the ileocecal
junction, the union of the terminal ileum and the cecum. Together, the jejunum and ileum
are 6-7 m long, the jejunum constituting approximately two
fifths and the ileum approximately three fifths of the intraperitoneal section of the small intestine.
Most of the jejunum lies in the left upper quadrant (LUQ)
of the infracolic compartment, whereas most of the ileum
lies in the right lower quadrant (RLQ). The terminal ileum
usually lies in the pelvis from which it ascends, ending in
the medial aspect of the cecum. Although no clear line of
demarcation between the jejunum and ileum exists, they
have distinctive characteristics that are surgically important.
The mesentery is a fan-shaped fold of peritoneum that
attaches the jejunum and ileum to the posterior abdominal
wall. The origin or root of the mesentery (approximately 15 cm long) is directed obliquely,
inferiorly, and to the right. It extends from
the duodenojejunal junction on the left side of vertebra L2to the ileocolic junction and the right sacro-iliac joint. The
average length of the mesentery from its root to the intestinal border is 20 cm. The root of the mesentery crosses
(successively) the ascending and inferior parts of the duodenum, abdominal aorta, IVC, right ureter, right psoas
major, and right testicular or ovarian vessels. Between the two layers of the mesentery are the superior mesenteric
vessels, lymph nodes, a variable amount of fat, and autonomic nerves.
The superior mesenteric artery (SMA) supplies the
jejunum and ileum via jejunal and ileal arteries.
The SMA usually arises from the abdominal aorta at the
level of the L1 vertebra, approximately 1 cm inferior to the celiac trunk, and runs between the layers of the mesentery,
sending 15-18 branches to the jejunum and ileum. The arteries unite to form loops or
arches, called arterial arcades, which give rise to straight
arteries, called vasa recta.
The superior mesenteric vein drains the jejunum and
ileum. It lies anterior and to the right of the
SMA in the root of the mesentery. The SMV
ends posterior to the neck of the pancreas, where it unites
with the splenic vein to form the hepatic portal vein.
Specialized lymphatic vessels in the intestinal villi (tiny
projections of the mucous membrane) that absorb fat are
called lacteals. They empty their milk-like fluid into the
lymphatic plexuses in the walls of the jejunum and ileum.
The lacteals drain in turn into lymphatic vessels between the
layers of the mesentery. Within the mesentery, the lymph
passes sequentially through three groups of lymph nodes:
• Juxta-intestinal lymph nodes: located close to the
intestinal wall.
• Mesenteric lymph nodes: scattered among the arterial
arcades.
• Superior central nodes: located along the proximal part
of the SMA.
Efferent lymphatic vessels from the mesenteric lymph nodes
drain to the superior mesenteric lymph nodes. Lymphatic vessels from the terminal ileum follow the ileal branch of the
ileocolic artery to the ileocolic lymph nodes.
The SMA and its branches are surrounded by a peri-arterial nerve plexus through which the nerves are conducted to the parts of the intestine supplied by this artery. The sympathetic fibers in the nerves to the jejunum and ileum originate in the T8-T10 segments of the spinal cord and reach the superior mesenteric nerve plexus
through the sympathetic trunks and thoracic abdominopelvic
(greater, lesser, and least) splanchnic nerves. The presynaptic sympathetic fibers synapse on cell bodies of postsynaptic
sympathetic neurons in the celiac and superior mesenteric
(prevertebral) ganglia. The parasympathetic fibers in the
nerves to the jejunum and ileum derive from the posterior
vagal trunks. The presynaptic parasympathetic fibers synapse
with postsynaptic parasympathetic neurons in the myenteric
and submucosal plexuses in the intestinal wall.
Sympathetic stimulation reduces peristaltic and secretory
activity of the intestine and acts as a vasoconstrictor, reducing or stopping digestion and making blood (and energy)
available for "fleeing or fighting." Parasympathetic stimulation increases peristaltic and secretory activity of the intestine, restoring the digestion process following a sympathetic
reaction. The small intestine also has sensory (visceral afferent) fibers. The intestine is insensitive to most pain stimuli,
including cutting and burning; however, it is sensitive to distension that is perceived as colic (spasmodic abdominal pains
or "intestinal cramps").