Main Model
11 Uterus
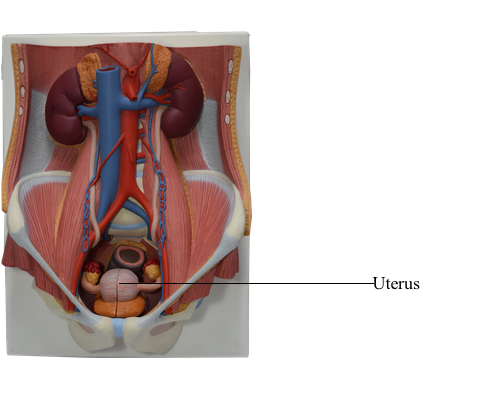
The uterus (womb) is a thick-walled, pear-shaped, hollow muscular organ. The embryo and fetus develop in the uterus. Its muscular walls adapt to the growth of the fetus and then provide the power for its expulsion during childbirth. The non-gravid (non-pregnant) uterus usually lies in the lesser pelvis, with its body lying on the urinary bladder and its cervix between the urinary bladder and rectum.
The uterus is a very dynamic structure, the size and proportions of which change during the various changes of life.
The adult uterus is usually anteverted (tipped anterosuperiorly relative to the axis of the vagina) and anteflexed (flexed or bent anteriorly relative to the cervix, creating the angle of flexion) so that its mass lies over the bladder. Consequently, when the bladder is empty, the uterus typically lies in a nearly transverse plane. The position of the uterus changes with the degree of fullness of the bladder and rectum, and stage of pregnancy. Although its size varies considerably, the non-gravid uterus is approximately 7.5 cm long, 5 cm wide, and 2 cm thick and weighs approximately 90 grams.
The uterus is divisible into two main parts: the body and cervix.
The body of the uterus, forming the superior two thirds of the organ, includes the fundus of the uterus, the rounded part that lies superior to the uterine ostia. The body lies between the layers of the broad ligament and is freely movable. It has two surfaces: vesical (related to the bladder) and intestinal. The body is demarcated from the cervix by the isthmus of the uterus, a relatively constricted segment, approximately 1 cm long.
The cervix of the uterus is the cylindrical, relatively narrow inferior third of the uterus, approximately 2.5 cm long in an adult non-pregnant woman. For descriptive purposes, two parts are described: a supravaginal part between the isthmus and the vagina, and a vaginal part, which protrudes into the superiormost anterior vaginal wall. The rounded vaginal part surrounds the external os of the uterus and is surrounded in turn by a narrow recess, the vaginal fornix. The supravaginal part is separated from the bladder anteriorly by loose connective tissue and from the rectum posteriorly by the recto-uterine pouch.
The slit-like uterine cavity is approximately 6 cm in length from the external os to the wall of the fundus. The uterine horns (Latin cornua) are the superolateral regions of the uterine cavity, where the uterine tubes enter. The uterine cavity continues inferiorly as the cervical canal. The fusiform canal extends from a narrowing inside the isthmus of the uterine body, the anatomical internal os, through the supravaginal and vaginal parts of the cervix, communicating with the lumen of the vagina through the external os. The uterine cavity (in particular, the cervical canal) and the lumen of the vagina together constitute the birth canal, through which the fetus passes at the end of gestation.
The wall of the body of the uterus consists of three coats, or layers:
• Perimetrium - the serosa or outer serous coat - consists of peritoneum supported by a thin layer of connective tissue.
• Myometrium - the middle coat of smooth muscle - becomes greatly distended (more extensive but much thinner) during pregnancy. The main branches of the blood vessels and nerves of the uterus are located in this coat. During childbirth, contraction of the myometrium is hormonally stimulated at intervals of decreasing length to dilate the cervical os and expel the fetus and placenta. During the menses, myometrial contractions may produce cramping.
• Endometrium - the inner mucous coat - is firmly adhered to the underlying myometrium. The endometrium is actively involved in the menstrual cycle, differing in structure with each stage of the cycle. If conception occurs, the blastocyst becomes implanted in this layer; if conception does not occur, the inner surface of this coat is shed during menstruation.
The amount of muscular tissue in the cervix is markedly less than in the body of the uterus. The cervix is mostly fibrous and is composed mainly of collagen with a small amount of smooth muscle and elastin.
Ligaments of Uterus
Externally, the ligament of the ovary attaches to the uterus postero-inferior to the uterotubal junction. The round ligament of the uterus (Latin ligamentum teres uteri) attaches antero-inferiorly to this junction. These two ligaments are vestiges of the ovarian gubernaculum, related to the relocation of the gonad from its developmental position on the posterior abdominal wall.
The broad ligament of the uterus is a double layer of peritoneum (mesentery) that extends from the sides of the uterus to the lateral walls and floor of the pelvis. This ligament assists in keeping the uterus in position. The two layers of the broad ligament are continuous with each other at a free edge that surrounds the uterine tube. Laterally, the peritoneum of the broad ligament is prolonged superiorly over the vessels as the suspensory ligament of the ovary. Between the layers of the broad ligament on each side of the uterus, the ligament of the ovary lies posterosuperiorly and the round ligament of the uterus lies antero-inferiorly. The uterine tube lies in the anterosuperior free border of the broad ligament, within a small mesentery called the mesosalpinx. Similarly, the ovary lies within a small mesentery called the mesovarium on the posterior aspect of the broad ligament. The largest part of the broad ligament, inferior to the mesosalpinx and mesovarium, which serves as a mesentery for the uterus itself, is the mesometrium.
The uterus is a dense structure located in the center of the pelvic cavity. The principal supports of the uterus holding it in this position are both passive and active or dynamic. Dynamic support of the uterus is provided by the pelvic diaphragm. Its tone during sitting and standing and active contraction during periods of increased intra-abdominal pressure (sneezing, coughing, etc.) is transmitted through the surrounding pelvic organs and the endopelvic fascia in which they are embedded. Passive support of the uterus is provided by its position - the way in which the normally anteverted and anteflexed uterus rests on top of the bladder. When intra-abdominal pressure is increased, the uterus is pressed against the bladder. The cervix is the least mobile part of the uterus because of the passive support provided by attached condensations of endopelvic fascia (ligaments), which may also contain smooth muscle:
• Cardinal (transverse cervical) ligaments extend from the supravaginal cervix and lateral parts of the fornix of the vagina to the lateral walls of the pelvis.
• Uterosacral ligaments pass superiorly and slightly posteriorly from the sides of the cervix to the middle of the sacrum; they are palpable during a rectal examination.
Together these passive and active supports keep the uterus centered in the pelvic cavity and resist the tendency for the uterus to fall or be pushed through the vagina.
Relations of Uterus
Peritoneum covers the uterus anteriorly and superiorly, except for the cervix. The peritoneum is reflected anteriorly from the uterus onto the bladder and posteriorly over the posterior part of the fornix of the vagina to the rectum. Anteriorly, the uterine body is separated from the urinary bladder by the vesico-uterine pouch, where the peritoneum is reflected from the uterus onto the posterior margin of the superior surface of the bladder. Posteriorly, the uterine body and supravaginal part of the cervix are separated from the sigmoid colon by a layer of peritoneum, and the peritoneal cavity and from the rectum by the recto-uterine pouch. Laterally, the uterine artery crosses the ureter superiorly, near the cervix.
Summary of the Relations of the Uterus:
• Anteriorly (antero-inferiorly in its normal anteverted position): the vesico-uterine pouch and superior surface of the bladder; the supravaginal part of the cervix is related to the bladder and is separated from it by only fibrous connective tissue.
• Posteriorly: the recto-uterine pouch containing loops of small intestine and the anterior surface of rectum; only the visceral pelvic fascia uniting the rectum and uterus here resists increased intra-abdominal pressure.
• Laterally: the peritoneal broad ligament flanking the uterine body and the fascial cardinal ligaments on each side of the cervix and vagina; in the transition between the two ligaments, the ureters run anteriorly slightly superior to the lateral part of the vaginal fornix and inferior to the uterine arteries, usually approximately 2 cm lateral to the supravaginal part of the cervix.
The blood supply of the uterus derives mainly from the uterine arteries, with potential collateral supply from the ovarian arteries.
The uterine veins enter the broad ligaments with the arteries and form a uterine venous plexus on each side of the cervix. Veins from the uterine plexus drain into the internal iliac veins.