Main Model
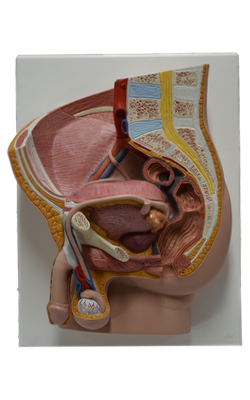
Sigmoid colon (pelvic colon)
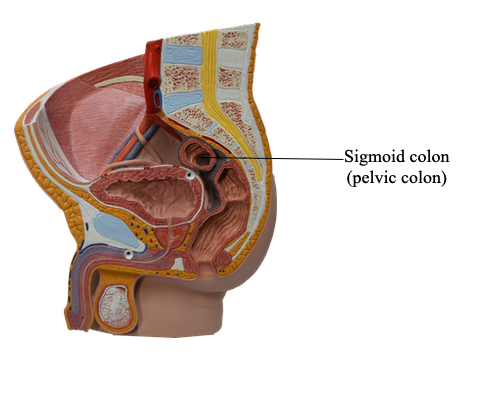
The sigmoid colon, characterized by its S-shaped loop of variable length, links the descending colon and the rectum. The sigmoid colon extends from the iliac fossa to the third sacral (S3) vertebra, where it joins the rectum. The termination of the teniae coli, approximately 15 cm from the anus, indicates the rectosigmoid junction.
The sigmoid colon usually has a long mesentery - the sigmoid mesocolon - and therefore has considerable freedom of movement, especially its middle part. The root of the sigmoid mesocolon has an inverted V-shaped attachment, extending first medially and superiorly along the external iliac vessels and then medially and inferiorly from the bifurcation of the common iliac vessels to the anterior aspect of the sacrum. The left ureter and the division of the left common iliac artery lie retroperitoneally, posterior to the apex of the root of the sigmoid mesocolon. The omental appendices of the sigmoid colon are long; they disappear when the sigmoid mesentery terminates. The teniae coli also disappear as the longitudinal muscle in the wall of the colon broadens to form a complete layer in the rectum.
The arterial supply of the sigmoid colon is from the left colic and sigmoid arteries, branches of the inferior mesenteric artery. Thus, at approximately the left colic flexure, a second transition occurs in the blood supply of the abdominal part of the alimentary canal: the superior mesenteric artery (SMA) supplying blood to that part orad (proximal) to the flexure (derived from the embryonic mid gut), and the inferior mesenteric artery (IMA) supplying blood to the part aborad (distal) to the flexure (derived from the embryonic hindgut). The sigmoid arteries descend obliquely to the left, where they divide into ascending and descending branches. The superior branch of the most superior sigmoid artery anastomoses with the descending branch of the left colic artery, thereby forming a part of the marginal artery.
Venous drainage from the sigmoid colon is provided by the inferior mesenteric vein, flowing usually into the splenic vein and then the hepatic portal vein on its way to the liver.
Lymphatic drainage from the sigmoid colon is conducted through vessels passing to the epicolic and paracolic nodes, and then through the intermediate colic lymph nodes along the left colic artery. Lymph from these nodes passes to the inferior mesenteric lymph nodes that lie around the inferior mesenteric artery (IMA). However, lymph from the left colic flexure may also drain to the superior mesenteric lymph nodes.
Orad (toward the mouth, or proximal) to the left colic flexure, sympathetic and parasympathetic fibers travel together from the abdominal aortic plexus via peri-arterial plexuses to reach the abdominal part of the alimentary tract; however, aborad (away from the mouth, or distal) to the flexure, they follow separate routes.
The sympathetic nerve supply of the sigmoid colon is from the lumbar part of the sympathetic trunk via lumbar (abdominopelvic) splanchnic nerves, the superior mesenteric plexus, and the peri-arterial plexuses following the inferior mesenteric artery and its branches.
The parasympathetic nerve supply is from the pelvic splanchnic nerves via the inferior hypogastric (pelvic) plexus and nerves, which ascend retroperitoneally from the plexus, independent of the arterial supply to this part of the gastrointestinal tract. Orad to the middle of the sigmoid colon, visceral afferents conveying pain sensation pass retrogradely with sympathetic fibers to thoracolumbar spinal sensory ganglia, whereas those carrying reflex information travel with the parasympathetic fibers to vagal sensory ganglia. Aborad to the middle of the sigmoid colon, all visceral afferents follow the parasympathetic fibers retrogradely to the sensory ganglia of spinal nerves S2-S4.