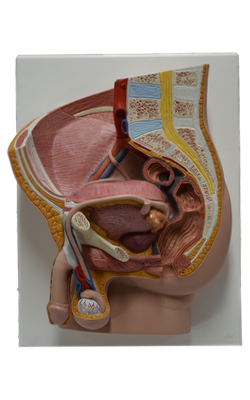
Main Model
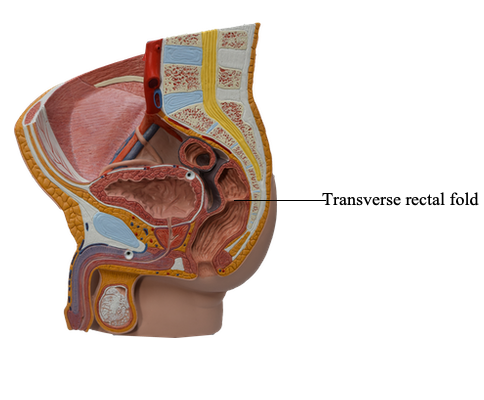
Transverse rectal fold
The rectum is the pelvic part of the digestive tract and is continuous proximally with the sigmoid colon and distally with the anal canal. The rectosigmoid junction lies anterior to the S3 vertebra. At this point, the teniae coli of the sigmoid colon spread to form a continuous outer longitudinal layer of smooth muscle, and the fatty omental appendices are discontinued.
Although its name is derived from the Latin term for “straight” (rectus), the term was coined during ancient studies on animals to describe the distal part of the colon; the human rectum is characterized by a number of flexures. The rectum follows the curve of the sacrum and coccyx, forming the sacral flexure of the rectum. The rectum ends anteroinferior to the tip of the coccyx, immediately before a sharp postero-inferior angle (the anorectal flexure of the anal canal) that occurs as the gut perforates the pelvic diaphragm (levator ani). The roughly 80° anorectal flexure is an important mechanism for fecal continence, being maintained during the resting state by the tonus of the puborectalis muscle, and by its active contraction during peristaltic contractions if defecation is not to occur. With the flexures of the rectosigmoid junction superiorly and the anorectal junction inferiorly, the rectum has an S shape when viewed laterally.
Three sharp lateral flexures of the rectum (superior and inferior on the left side, and intermediate on the right) are apparent when the rectum is viewed anteriorly. The flexures are formed in relation to three internal infoldings (transverse rectal folds): two on the left and one on the right side. The folds overlie thickened parts of the circular muscle layer of the rectal wall. The dilated terminal part of the rectum, lying directly superior to and supported by the pelvic diaphragm (levator ani) and anococcygeal ligament, is the ampulla of the rectum. The ampulla receives and holds an accumulating fecal mass until it is expelled during defecation. The ability of the ampulla to relax to accommodate the initial and subsequent arrivals of fecal material is another essential element of maintaining fecal continence.
Peritoneum covers the anterior and lateral surfaces of the superior third of the rectum, only the anterior surface of the middle third, and no surface of the inferior third because it is subperitoneal. In males, the peritoneum reflects from the rectum to the posterior wall of the bladder, where it forms the floor of the rectovesical pouch. In females, the peritoneum reflects from the rectum to the posterior part of the fornix of the vagina, where it forms the floor of the recto-uterine pouch. In both sexes, lateral reflections of peritoneum from the superior third of the rectum form pararectal fossae, which permit the rectum to distend as it fills with feces.
The rectum lies posteriorly against the inferior three sacral vertebrae and the coccyx, anococcygeal ligament, median sacral vessels, and inferior ends of the sympathetic trunks and sacral plexuses. In males, the rectum is related anteriorly to the fundus of the urinary bladder, terminal parts of the ureters, ductus deferentes, seminal glands, and prostate. The rectovesical septum lies between the fundus of the bladder and the ampulla of the rectum and is closely associated with the seminal glands and prostate. In females, the rectum is related anteriorly to the vagina and is separated from the posterior part of the fornix and the cervix by the recto-uterine pouch. Inferior to this pouch, the weak rectovaginal septum separates the superior half of the posterior wall of the vagina from the rectum.
The superior rectal artery, the continuation of the abdominal inferior mesenteric artery, supplies the proximal part of the rectum. The right and left middle rectal arteries, which often arise from the anterior divisions of the internal iliac arteries in the pelvis, supply the middle and inferior parts of the rectum. The inferior rectal arteries, arising from the internal pudendal arteries in the perineum, supply the anorectal junction and anal canal. Anastomoses between the superior and inferior rectal arteries may provide potential collateral circulation, but anastomoses with the middle rectal arteries are sparse.
Blood from the rectum drains through the superior, middle, and inferior rectal veins. Anastomoses occur between the portal and systemic veins in the wall of the anal canal. Because the superior rectal vein drains into the portal venous system and the middle and inferior rectal veins drain into the systemic system, these anastomoses are clinically important areas of portocaval anastomosis. The submucosal rectal venous plexus surrounds the rectum, communicating with the vesical venous plexus in males and the uterovaginal venous plexus in females. The rectal venous plexus consists of two parts: the internal rectal venous plexus just deep to the mucosa of the anorectal junction and the subcutaneous external rectal venous plexus external to the muscular wall of the rectum. Although these plexuses bear the term rectal, they are primarily “anal” in terms of location, function, and clinical significance.
The nerve supply to the rectum is from the sympathetic and parasympathetic systems. The sympathetic supply is from the lumbar spinal cord, conveyed via lumbar splanchnic nerves and the hypogastric/ pelvic plexuses, and through the peri-arterial plexus of the inferior mesenteric and superior rectal arteries. The parasympathetic supply is from the S2-S4 spinal cord level, passing via the pelvic splanchnic nerves and the left and right inferior hypogastric plexuses to the rectal (pelvic) plexus. Because the rectum is inferior (distal) to the pelvic pain line, all visceral afferent fibers follow the parasympathetic fibers retrogradely to the S2-S4 spinal sensory ganglia.