Main Model
Sphincter ani internus muscle

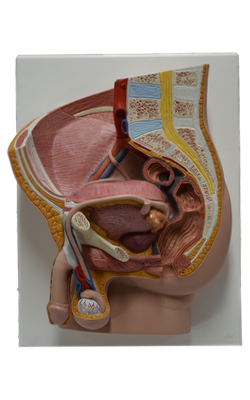
The anal canal is the terminal part of the large intestine and of the entire digestive tract. It extends from the superior aspect of the pelvic diaphragm to the anus. The canal (2.5-3.5 cm long) begins where the rectal ampulla narrows at the level of the U-shaped sling formed by the puborectalis muscle. The anal canal ends at the anus, the external outlet of the alimentary tract. The anal canal, surrounded by internal and external anal sphincters, descends postero-inferiorly between the anococcygeal ligament and the perineal body. The canal is collapsed, except during passage of feces. Both sphincters must relax before defecation can occur.
The internal anal sphincter is an involuntary sphincter surrounding the superior two thirds of the anal canal. It is a thickening of the circular muscle layer. Its contraction (tonus) is stimulated and maintained by sympathetic fibers from the superior rectal (peri-arterial) and hypogastric plexuses. Its contraction is inhibited by parasympathetic fiber stimulation, both intrinsically in relation to peristalsis, and extrinsically by fibers conveyed by the pelvic splanchnic nerves. This sphincter is tonically contracted most of the time to prevent leakage of fluid or flatus; however, it relaxes (is inhibited) temporarily in response to distension of the rectal ampulla by feces or gas, requiring voluntary contraction of the puborectalis and external anal sphincter if defecation or flatulence is not to occur. The ampulla relaxes after initial distension (when peristalsis subsides) and tonus returns until the next peristalsis, or until a threshold level of distension occurs, at which point inhibition of the sphincter is continuous until distension is relieved.
The external anal sphincter is a large voluntary sphincter that forms a broad band on each side of the inferior two thirds of the anal canal. This sphincter is attached anteriorly to the perineal body and posteriorly to the coccyx via the anococcygeal ligament. It blends superiorly with the puborectalis muscle.
The external anal sphincter is described as having subcutaneous, superficial, and deep parts; these are zones rather than muscle bellies and are often indistinct. The external anal sphincter is supplied mainly by S4 through the inferior rectal nerve, although its deep part also receives fibers from the nerve to the levator ani, in common with the puborectalis, with which it contracts in unison to maintain continence when the internal sphincter is relaxed (except during defecation).
Internally, the superior half of the mucous membrane of the anal canal is characterized by a series of longitudinal ridges called anal columns. These columns contain the terminal branches of the superior rectal artery and vein. The anorectal junction, indicated by the superior ends of the anal columns, is where the rectum joins the anal canal. At this point, the wide rectal ampulla abruptly narrows as it traverses the pelvic diaphragm. The inferior ends of the anal columns are joined by anal valves. Superior to the valves are small recesses called anal sinuses. When compressed by feces, the anal sinuses exude mucus, which aids in evacuation of feces from the anal canal.
The inferior comb-shaped limit of the anal valves forms an irregular line, the pectinate line, that indicates the junction of the superior part of the anal canal (visceral; derived from the embryonic hindgut), and the inferior part (somatic; derived from the embryonic proctodeum).
The anal canal superior to the pectinate line differs from the part inferior to the pectinate line in its arterial supply, innervation, and venous and lymphatic drainage. These differences result from the different embryological origins of the superior and inferior parts of the anal canal.
The superior rectal artery supplies the anal canal superior to the pectinate line. The two inferior rectal arteries supply the anal canal inferior to the pectinate line as well as the surrounding muscles and peri-anal skin. The middle rectal arteries assist with the blood supply to the anal canal by forming anastomoses with the superior and inferior rectal arteries.
The internal rectal venous plexus drains in both directions from the level of the pectinate line. Superior to the pectinate line, the internal rectal plexus drains chiefly into the superior rectal vein (a tributary of the inferior mesenteric vein) and the portal system. Inferior to the pectinate line, the internal rectal plexus drains into the inferior rectal veins (tributaries of the caval venous system) around the margin of the external anal sphincter. The middle rectal veins (tributaries of the internal iliac veins) mainly drain the muscularis externa of the ampulla and form anastomoses with the superior and inferior rectal veins. In addition to the abundant venous anastomoses, the rectal plexuses receive multiple arteriovenous anastomoses (AVAs) from the superior and middle rectal arteries.
The normal submucosa of the anorectal junction is markedly thickened, and in section has the appearance of a cavernous (erectile) tissue, owing to the presence of the sacculated veins of the internal rectal venous plexus. The vascular submucosa is especially thickened in the left lateral, right anterolateral, and right posterolateral positions, forming anal cushions, or threshold pads, at the point of closure of the anal canal. Because these cushions contain plexuses of saccular veins capable of directly receiving arterial blood via multiple AVAs, they are variably pliable and turgid, and form a sort of flutter valve that contributes to the normally water- and gas- tight closure of the anal canal.
Superior to the pectinate line, the lymphatic vessels drain deeply into the internal iliac lymph nodes, and through them into the common iliac and lumbar lymph nodes. Inferior to the pectinate line, the lymphatic vessels drain superficially into the superficial inguinal lymph nodes, as does most of the perineum.
The nerve supply to the anal canal superior to the pectinate line is visceral innervation from the inferior hypogastric plexus, involving sympathetic, parasympathetic, and visceral afferent fibers. Sympathetic fibers maintain the tonus of the internal anal sphincter. Parasympathetic fibers inhibit the tonus of the internal sphincter and evoke peristaltic contraction for defecation. The superior part of the anal canal, like the rectum superior to it, is inferior to the pelvic pain line; all visceral afferents travel with the parasympathetic fibers to spinal sensory ganglia S2-S4. Superior to the pectinate line, the anal canal is sensitive only to stretching, which evokes sensations at both the conscious and unconscious (reflex) levels. For example, distension of the rectal ampulla inhibits (relaxes) the tonus of the internal sphincter.
The nerve supply of the anal canal inferior to the pectinate line is somatic innervation derived from the inferior anal (rectal) nerves, branches of the pudendal nerve. Therefore, this part of the anal canal is sensitive to pain, touch, and temperature. Somatic efferent fibers stimulate contraction of the voluntary external anal sphincter.